Operative choices
When operations are planned on the bony skeleton, the following broad categories
of operations are available. Factors such as age and physical fitness are
important in making the choice regarding the most appropriate procedure
Osteotomies
An osteotomy is the section and realignment of a bone. This realigns the
bone and may be used to correct an existing deformity e.g. varus of the
tibia. Realignment also redistributes the forces over a joint and a normal
area of the joint can be loaded in preference to the pathological e.g. osteoarthritic
areas.
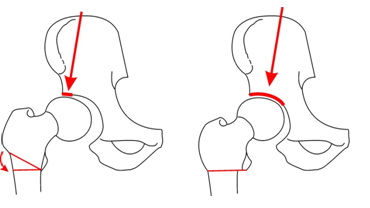
Hip Osteotomy
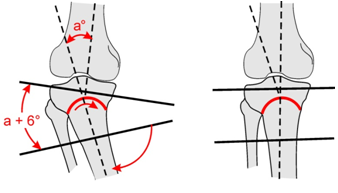 |
| Maquet proximal tibial
osteotomy |
Indications Osteotomy
- Age - young
- Mal alignment
- Mobile joint
Contraindications
- Immobile joint
- Poliarthritis
Arthrodesis
The joint is surgically fused in a position of function. Arthrodeses are
usually indicated in the younger patient with mono arthritis. E.g. Posttraumatic
osteoarthritis of the hip in a 20 year old active patient.
Indications Arthrodesis
- Young patient
- Severe pain
- Loss of joint motion
Contraindications hip Arthrodesis
- Ipsilateral knee pathology
- Other hip affected
- Lumbar spine pathology
 A hip arthrodesis would be contraindicated in avascualar
necrosis of the hip caused by alcohol or steroids as there is a high chance
the other hip will develop AVN too. A hip arthrodesis would be contraindicated in avascualar
necrosis of the hip caused by alcohol or steroids as there is a high chance
the other hip will develop AVN too.
Excision Arthroplasty
The joint is excised on one or both sides. Examples are the Girdlestone
arthroplasty of the hip. Here the femur head and neck are excised. A Keller's
operation of the first MP Joint of the big toe was a popular operation for
hallux valgus with joint degeneration. The proximal end of the first phalanx
was excised.
 |
|
Keller excision arthroplasty for hallux valgus
|
 |
Girdlestone Excision Arthroplasty
Necessitated by sepsis - note the Gentamycin beads |
Indications Girdlestone
- Sepsis e.g. septic hip replacement.
- Older patient.
Girdlestone operations are rarely done these days, but are a choice where
sepsis precludes total hip replacement. They leave a mobile joint but always
result in some shortening of the femur and are never entirely pain free.
Joint Replacement
Joint replacement is a cost-effective way of rehabilitating a patient with
arthritis of the hip, knee and even shoulder.
 |
Moore's prosthesis
Un cemented femoral component Acetabulum is not replaced. Indication
- intra capsular fracture in the elderly |
Types of joint replacement
- Hemi replacement e.g. Moore's prosthesis
- Total joint replacement
The “Gold Standard” is a cemented hip.
In the active younger patient an un cemented component may be used so
that bone stock is preserved for a later revision. At present a hip replacement
should last 15 or more years before a revision is needed.
Indications Total Hip
- Age > 60 yr
- Grade 3 pain or more
- Limited walking distance
Contraindications Total Hip
- Any sepsis
- Age < 60 yr (except rheumatoid)
- Neuromuscular disease
 
Hip Pain: Decisions as to type of operation
An adolescent or child can be offered a osteotomy if the hip has more than
60 degrees of flexion. In severe hip osteoarthritis at this age, an arthrodesis
is still a good choice. Between the ages of 30 and 55 years total hip replacements
for OA are best avoided. Continue with conservative treatment if possible.
An osteotomy can be considered if there is hip motion and a normal area
of cartilage than can be moved into the superior weight bearing area by
an osteotomy.
In the active older patient a total hip replacement is the ideal treatment
for osteoarthritis. Because patients with autoimmune diseases such as
Rheumatoid arthritis have limited mobility, a total hip replacement can
be done at any age.
|