Tendon Transfer
Loss of movement due to paralysis can sometimes be restored using a piece
of tendon/ muscle unit whose function can be spared.
Pre-requites for a successful tendon transfer
- Stability of proximal joints
- Prior correction of any fixed deformity
- At least grade 4/5 power
- Direct line of pull
- Firm point of fixation - preferably bone
Joint mobility is maintained pre-operatively by physiotherapy.
There can be no fixed contractures. Postoperatively the joint is splinted
for at least six weeks.
| 
|
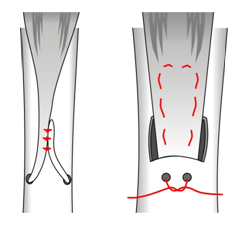
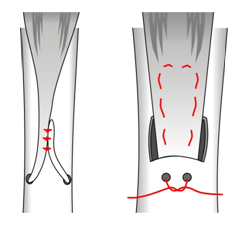
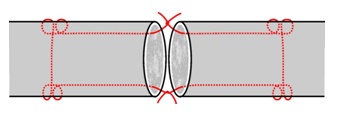
| Methods of attaching
tendon to bone |
The best way of attaching tendon to bone is to drill a tunnel through
the bone and loop the tendon back onto itself and then suture the tendon
to itself.
Suture of tendons
| 
|
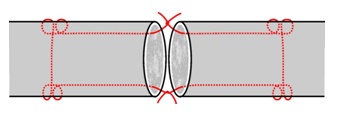
| Kessler suture
for hand flexor tendons |
Severed tendons are best sutured primarily. In some situations such
as Zone 2 (under the flexor pulleys in the palm) special suture
techniques such as the Kessler suture allow a less bulky suture line.
Nerve Repair
Classification of nerve damage
- Neurotmesis (complete division) Usually seen in open wounds
e.g. knife wound. The nerve is completely severed.
- Axonotmesis (incomplete division) Only the axoms are divided.
Usually in traction and closed injuries. Clinically it in indistinguishable
from axomomesis, but complete recovery is likely
- Neurapraxia (physiological interruption) The axoms are
intact and the only injury is degradation of the axon sheaths. Motor
loss is usually seen and sensory loss is less common.
Nerve Suture
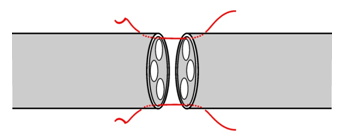
| 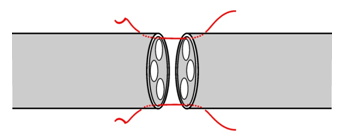
|
| Nerve Suture. Fascicles are matched
and epineuruim sutured with 6/0 or finer material |
Timing of repair
- Immediate exploration and suture of open injuries
- Closed nerve
injuries can be treated conservatively (i.e. splints and physiotherapy)
and observed for signs of recovery. Repair is undertaken at 6 weeks
to a few months later if necessary.
Signs of nerve recovery
- Return of sensory or motor function
- Progressive Tinnel
sign ( point of percussion tenderness over nerve course)
migration distally.
- Speed of growth about 6mm per week. The distance to the target organ
is thus critical. The higher the lesion, the worse the prognosis.
<< Index Page |