Fractures of the proximal tibia that break into the knee are known as plateau fractures. They are often displaced. Open reduction is often required because of this and there is a real risk of skin breakdown and sepsis because of the subcutaneous nature, and poor blood supply of this region
Classification
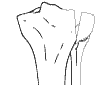 |
Schatzker 1: Split Fracture of the lateral side. Seen in younger patients. Ligamentous disruptions are common in this group. Meniscal injuries are common. |
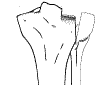 |
Schatzker 2: Depressed fracture of the lateral side with central depression |
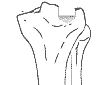 |
Schatzker 3: A depressed -central or lateral fracture with no split component. Lower energy fracture - usually in older persons. |
 |
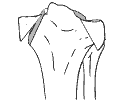
Schatzker 4: Medial Depression - no split. Often seen in elderly patients. Peroneal nerve injury is common due to traction on the medial side. |
 |
Schatzker 5: Bicondylar. Split fractures, no depression, Shaft still connects to medial portion |
 |
Schatzker 6: Bicondylar with associated shaft fracture. Because it is high energy, popliteal injury is common. |
As can be seen from the above ligamentous and meniscal injuries are common, especially in the younger patient having a high velocity fracture. More severe forms such as the Schatzker 6 also have a high incidence of arterial injuries including compartment syndrome.
Management
Conservative management consists of skin or skeletal traction via a Den ham pin through the distal tibia or calcaneus. Alignment must be restored and this may entail a manipulation under anesthetic. The knee is mobilsed by the physiotherapist. Undisplaced or minimally displaced plateau fractures that do not have any depression are suitable for this treatment. Once the knee has gained 90 degrees flexion an above knee plaster cast may be applied until union in about six weeks.
All displaced fractures, especially those have depression require operative treatment. The optimal time is not immediately, swelling must first be treated by elevation, ice packs etc and definitive operation deferred until swelling subsides (in about a week). Obtain computer tomogrammes to visuaise the fracture in three dimensions and plan the operation.
Pure split type fractures may be treated by arthroscopy to visualise the fracture and per cutaneous screwing. Fluoroscopy and per cutaneous pinning also may be done if there is no depression and the fracture can be reduced easily.
 |
| Schatzker 5 fracture fixed with
per cutaneous screws Click on image for more views |
Most other plateau fractures need open reduction and internal fixation. The split part of fracture is visualised and opened up, the depressed area will need careful elevation and support from below by means of an autologous bone graft. The condyle is supported by means of a buttress plate and screws. Avoid bilateral plates - the extensive soft tissue swelling will lead to skin slough and sepsis. In Schatzker 5 fractures, open the worst side and elevate it with a buttress plate. The proximal screws are crossed over to support the far condyle. A locked plate is valuable in this situation as the (fixed to plate) proximal screws will prevent the far side migrating downwards.
 |
| Schatzker 1 fracture fixed with buttress plate and locking screws. Click to see the preoperative image |
In Schatzker 6 fractures internal fixation is risky and an Ilizarov external fixation (with pins no closer than 1.5 cm from the knee joint line) can be used. Another method of avoiding massive soft tissue swelling is to do ORIF with the plate placed subcutaneously. The screws are inserted using fluoroscopy, using a small stab incision over the screw hole.