Polio in SA: Assessing the risks
Engela Duvenage

An illustration depicts a polio virus particle

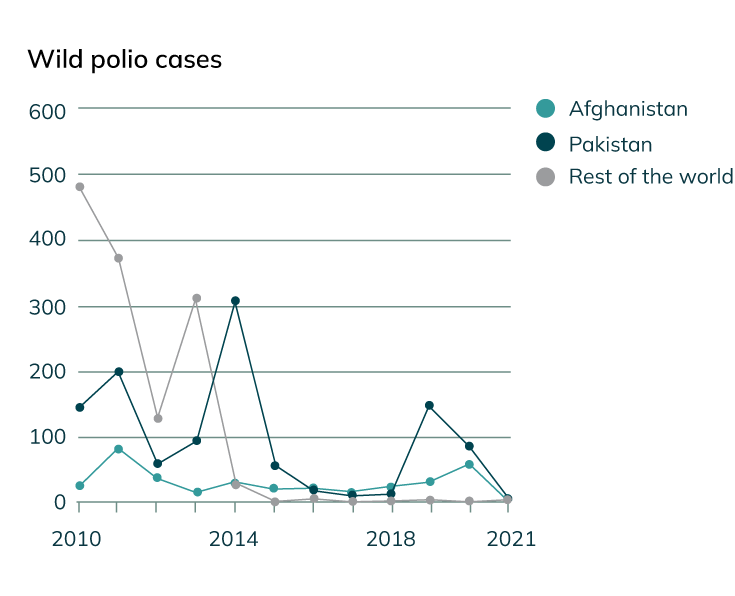
In her 2020 book Outbreaks and Epidemics, science journalist and CNN health editor Meera Senthilingam described how the worldwide polio eradication programme had managed to reduce the global number of cases from 350 000 in 1988 to only a handful at the time of print.
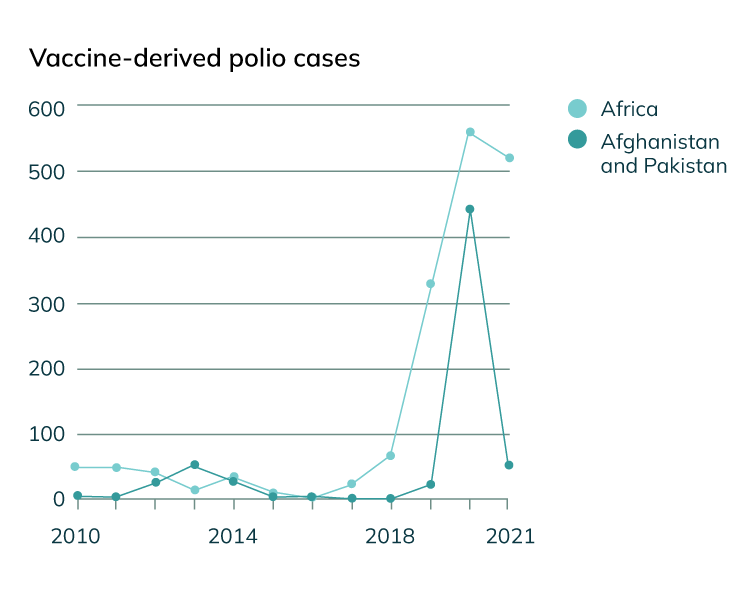
She explained that two of the three immunologically unique strains of wild (naturally occurring) poliovirus were certified as having been eradicated: type 2 in 2015 and type 3 in 2019.
Regarding a third wild type, WPV1, she noted: “Wild poliovirus type 1, still circulating in Pakistan and Afghanistan – no new cases have been detected on the African continent since 2016 – is the final hurdle.”
Unfortunately, this optimism about the situation in Africa was short-lived: six cases of WPV1 were reported in sub-Saharan Africa by mid-2022, one in Malawi and the rest in Mozambique. These cases were noted after the patients suddenly experienced some form of paralysis or weakness in their limbs (in medical terms, ‘acute flaccid paralysis’ or ‘AFP’).
Also in 2022, the USA, Israel, Yemen, the UK and 11 African countries reported cases of circulating vaccine-derived poliovirus 2 (cVDPV2). Albeit extremely rare, this strain can spread from someone who has been vaccinated to individuals in undervaccinated communities who have not received protection.
Smartening up to see the bigger picture
“Given that AFP cases represent only roughly 1 in 200 WPV1 infections, the cases observed in Malawi and Mozambique may suggest widespread circulation of the virus in the southern African region,” warns epidemiologist Prof Juliet Pulliam, director of the DSI-NRF Centre of Excellence in Epidemiological Modelling and Analysis (SACEMA) at Stellenbosch University.
Consequently, SACEMA’s Modelling and Analysis Response Team (SMART) has launched a modelling project to help health authorities keep their fingers on the pulse of potential polio outbreaks in Southern Africa.
SMART will also determine the value and input of potential preventative measures and/or interventions, in collaboration with the National Institute for Communicable Diseases (NICD).
“We have begun to develop a transmission-dynamic model of what poliovirus circulation could look like if the virus were introduced into South Africa,” says Pulliam, leader of SMART.
The team’s work can be used to project the time it would likely take between the introduction of the poliovirus and its detection on grounds of AFP cases.
The team also plans to take stock of the impact of reactive vaccination programmes put in place when polio cases emerge, and to assess the efficacy of these programmes depending on timely implementation. They will then compare the relative success of reactive vaccination to that of pre-emptively giving people extra doses of the polio vaccine to keep the number of infections to the absolute minimum.
“Our model will be run for specific populations, based on a characterisation of its age structure and vaccine coverage, and on how efficiently surveillance is being done in a given area.”
“We hope this work will encourage the government to act quickly towards reducing the polio risk,” Pulliam notes.
Mathematical models inform epidemic responses
The World Health Organization (WHO) warns that as long as a single child is infected with the poliovirus, children in all countries remain at risk. Unless the virus is eradicated from its last remaining strongholds, we may still see a global resurgence of the disease, they caution.
In 2020, the WHO unfortunately had to adjust its worldwide polio eradication programme in order to address the COVID-19 pandemic that was sweeping across the globe. This resulted in various polio vaccination activities being postponed for months. In the African region, 60% to 70% of the WHO’s resources earmarked for the polio eradication programme were reassigned towards fighting the pandemic.
According to Pulliam, SMART will be using many of the valuable techniques, best practices and lessons they have learned from modelling the COVID-19 pandemic and other diseases such as HIV and malaria in times of crisis.
“Mathematical models remain a really important tool for epidemic response,” she says. “In some contexts, they are the only way to ask questions about the potential impacts of different factors," Pulliam says.
“Any time someone makes a prediction or advocates for one intervention over another, there’s a mental model being used to back up what they’re saying. The value of mathematical modelling is that it makes those assumptions explicit. It formalises it, seeing as it’s a formal tool for making predictions and comparisons.
“It helps us think more clearly about what’s happening.
“We cannot change a weather prediction with our actions. We can be prepared and take an umbrella, but we can’t say that we don’t want a hurricane to come. But in epidemics, you can actually change the outcome by using interventions that make a difference.”
POLIO FACTS
Polio (poliomyelitis) is a highly infectious disease caused by a virus.
One in every 200 infections leads to irreversible paralysis.

Children under the age of five years are the most vulnerable.
Up to 10% of paralysed patients die because they struggle to breathe when their breathing muscles become affected.
Cases caused by wild poliovirus decreased by over 99% from an estimated 350 000 cases in 1988 to 140 in 2020.
Only 5 cases were reported in 2021, all in Afghanistan and Pakistan, where the virus is endemic. Thus far in 2022, 6 cases have been reported in Africa, 20 in Pakistan and 2 in Afghanistan.