Scaphoid Fractures
Department of Orthopaedic Surgery - University Stellenbosch, South Africa
| Scahoid fractures - Management and Complications |
by
Dr. Johan Davis
1)
General
a. 50-80
% of carpal injuries
b. Most
commonly in young adult males 15-40 (rare under 10 years)
c. Anatomy
of the Scaphoid:
i. Divided
1. Proximal
pole
2. Distal
pole
3. Tubercle
4. Waist
ii. 80
% of surface covered in cartilage
iii. Ligamentous
attachments
1. Radioscaphocapitate
ligament (variable attachment to ulnar aspect of Scaphoid waist)
2. Dorsal
intercarpal ligament (provides primary vascular supply)
iv. Blood
supply (Gelbermann)
1. Major
supply derived from Scaphoid branches of Radial artery - enters dorsal
ridge.
Provides
70-80 % of supply, including supply to proximal pole
2. Distal
aspect supplied through branches entering the tubercle (supplies distal
30 %)
3. Fractures
at waist or proximal third - union required for revascularization
v. Kinematics
1. Global
wrist motion - flexion, extension, radioulnar deviation (radiocarpal
joint) and axial rotation around distal radioulnar joint
2. Forearm
responsible for 140 degrees of rotation
3. Radiocarpal
joint (primarily flexion and extension) 70 degrees in equal proportions,
radial deviation 20 degrees and ulnar deviation of 40 degrees
4. Radiocarpal
articulation acts as universal joint, allowing small degree of intercarpal
motion related to rotation of individual carpals
5. Dart-throwing
motion (DTM)
Functional
oblique wrist motion, from radial extension to ulnar flexion
Used
for most activities of daily living (plane may vary between activities
and individuals)
Mid-carpal
joint utilized
Less
Scaphoid and Lunate motion then with pure flexion-extension or radio-ulnar
deviation
DTM
generated by flexor carpi ulnaris and extensor carpi radiais brevis
and - longus, and further guided by extensor carpi ulnaris, and flexor
carpi radialis
Hammering or clubbing utilizes DTM with greater resultant arc of wrist motion then pure flexion extension.
|
|
||
|
DTM allows upper extremity to coil into cocking position and continuously extend during a power swing
DTM at a plane 30-45 degrees from sagittal plane allows functional wrist motion while minimizing radiocarpal motion - rehabilitation application
6. Scaphoid rests on the radioscaphocapitate ligament at its waist: using the ligament as an axis it rotates from a volar flexed perpendicular position, to a dorsiflexed longitudinal position vi. Pathomechanics
1. Radius, Lunate and Capitate classically described as a central link that is co-linear in the sagittal plane.
2. Scaphoid serves as a connecting strut - any flexion moment across the Scaphoid is balanced by an extension moment at the Triquetrum.
3. With destabilization of the Scaphoid (fracture or Scapho-lunar ligament disruption) the Lunate and Triquetrum assume a position of excessive dorsiflexion (Dorsal intercalated segmental instability [DISI]) - Scapholunate angle > 70 degrees
4. When the Triquetrum is destabilized (usually disruption of Lunotriquetral ligament complex) the intercalated lunate segment flexes (Volar intercalated segmental instability [VISI])
|
||
|
|
||
|
|
||
|
|
||
|
Artist representation of Radius-Lunate-Capitate link system with stabilizer (Scaphoid / Triquetrum)
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
2) Injury mechanism
a. Fall onto outstretched hand
b. Forced dorsiflexion (usually beyond 95 degrees extension), radially deviated wrist with intercarpal supination.
When wrist is extended >95 degrees, proximal pole of Scaphoid is held in a vice between Capitate and dorsal lip of Radius, and taut palmar capsule - distal pole still free to move with failure of Scaphoid at point receiving highest bending moment (Chao 1978)
c. Palmar flexion in 3 % of cases (Leslie & Dickenson; Clay et al)
3) Clinical evaluation (high diagnostic sensitivity, specificity approaches 74-80 %)
a. Wrist pain
b. Swelling and fullness off anatomical snuffbox - indicates effusion
c. Tender palpation of Scaphoid tubercle and anatomical snuffbox
d. Pronation followed by ulnar deviation cause pain
e. Slight reduction in range of motion
f. Reduced grip strength
g. Provocative tests
i. Scaphoid lift test: painful dorsal and volar ballottement
ii. Watson test: painful dorsal Scaphoid displacement as the wrist is moved from ulnar to radial deviation with compression of the tuberosity
iii. Scaphoid compression test: longitudinal force along 1 metacarpal elicits pain
iv. Resisted pronation causes pain
|
||
|
|
||
 ~ The patient moves the wrist from ulnar to radial deviation while the examiner applies pressure at the scaphoid tubercle.
Scaphoid Shift Test (Watson Test)
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
4) Differential diagnosis
a. Scapholunate instability
b. Lunate dislocation
c. Flexor carpi radialis tendon rupture
d. Radial styloid fracture
e. Trapezium fracture
f. De Quervain disease
g. 1st Carpometacarpal joint arthrosis
5) Radiographic evaluation (70 % sensitivity)
a. Standard PA
b. Lateral (wrist neutral)
c. 45 degree pronated oblique (STTJ)
d. 45 degree supinated oblique (Radio-scaphoid joint)
e. Scaphoid view (PA with ulnar deviation)
f. Others:
i. PA with wrist in slight extension (Ziter view)
ii. AP with clenched fist to detect a ligamentous injury
Initial films non-diagnostic in 15-25 % of cases.
6) Other special investigations
a. Technetium bone scan (92-95 % sensitivity; 60-95 % specificity)
b. MRI (90-100 % sensitivity; 90% specificity - false positives because of bone bruises)
i. Has ability to identify other sources of pain - ligamentous injury
ii. Expensive
iii. Less readily available
iv. May not demonstrate fracture displacement
c. CT
i. Less costly and readily available
ii. Clearer visualization of fracture displacement
iii. Frequent false positives when used for triage of non-displaced Scaphoid fractures -misinterpretation of vascular foramina or other normal lines
iv. Good for ruling out displacement, not for diagnosis (pre-operative planning)
d. Ultrasound evaluation
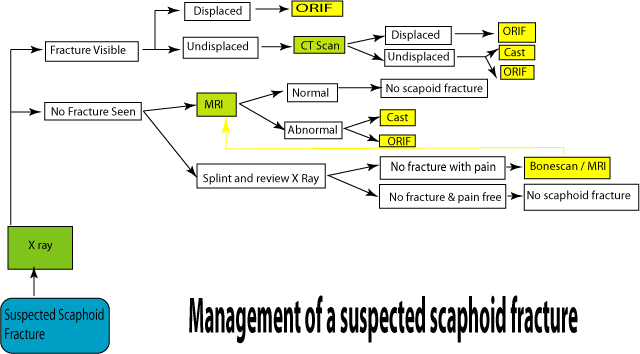
7) Diagnosis algorithm
|
||
|
|
||
|
||
|
|
||
|
|
||
|
|
||
|
|
|||
|
8) Classification
|
|||
|
|
|||
|
I. Russe classification of Scaphoid fractures:
|
|||
|
|
|||
|
Fracture pattern based
|
|||
|
|
|||
 |
|||
|
|
|||
|
Horizontal oblique (HO) 35 %, Transverse (T) 60 %, Vertical oblique (VO) 5 %
|
|||
|
|
|||
|
II. Herbert classification of Scaphoid fractures:
Displacement based (stable or unstable)
|
|||
|
|
|||
|
a.
|
 |
||
|
|
|||
|
|
|||
|
|
|||
|
|
||
|
III. Based on location
|
||
|
|
||
|
a. Tuberosity : 17-20 %
b. Distal pole : 10-12 %
c. Waist : 66-70 %
i. Horisontal oblique: 13-14 %
ii. Vertical oblique: 8-9 %
iii. Transverse: 45-48 %
d. Proximal pole 5-7 %
9) Treatment
a. Non-operative treatment (85-90 % of Scaphoid fractures will unite without surgical intervention (NJ Barton & TRC Davis 1999))
i. Indications:
1. Non-displaced distal third fractures
2. Tuberosity fractures
ii. Method
1. Cast immobilization
Inclusion of elbow?
i. Verdan 1960 - cadaver study: Supination of forearm causes shearing movement at fracture site.
ii. Falkenberg 1985 - cadaver study: X-fix from metacarpals to radius; supination of forearm causes no movement at fracture site
iii. Kuhlmann et al 1987 - cadaver study: Above elbow cast - harmful; blocked normal rotation of forearm bones, and any rotational movement made by patient transfers forces onto radio-carpal joint, with movement at fracture site.
iv. Advocates for above elbow casts, claiming superior results included -Verdan 1960, Broome et al 1964, Thomaidis 1973, Gellman et al 1989 (Gellman et al -Small randomized prospective study)
v. Below elbow cast as effective - Goldman et al 1969, Lindstrom 1975, Eddeland et al 1975, Alho and Kankaanpaa 1975
vi. Petracic 1985 used a hinged cast-brace to allow elbow movement, but prevent forearm rotation.
vii. Terkelsen and Jepsen 1988 - below elbow orthoplast brace as effective
Inclusion of the thumb?
i. Bohler senior 1920-1942 utilized an unpadded dorsal backslab, in 1942 started including the thumb (proximal phalanx)
ii. Idea of thumb proximal phalanx inclusion reinforced by Stewart 1954
iii. Soto-Hall included the distal phalanx to immobilize the IPJ as well (cadaver study showed FPL tendon pull caused movement at fracture)
iv. Yanni et al 1991, found that if the wrist was neither ulnar-deviated nor extended, the position of the thumb had no influence on the fracture gap
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
v. Clay et al 1991, large randomized prospective study - no difference in union rate whether thumb immobilized, or not - advocates a "Colles" type of cast with the thumb free (also recommended by Herbert 1990)
Inclusion of other fingers?
i. Dehne et al 1954 immobilized thumb, index and middle fingers
ii. Taleisnik 1985 recommended finger immobilization for potentially unstable fractures in good alignment, and early post surgery for nonunions
iii. Russe 1960 used a fist cast for vertical oblique fractures, preventing all finger movements (Taleisnik 1985; found hygiene unacceptable with this method)
Position of immobilization
i. If above elbow cast is used, most convenient position is agreed at 90 degrees of flexion
ii. Thomaidis 1973, and Gellman et al 1989; recommended neutral position in terms of forearm rotation
iii. In terms of wrist position - myriad of opinions and trials with varying conclusions
iv. Taleisnik 1985 - immobilization itself is important rather then position
v. Hambridge et al 1999 - Colles type POP in 20 degrees flexion compared to 20 degrees extension, 89 % union in both groups; 6 month follow up showed restriction in wrist extension in group treated with 20 degrees flexion casts
Material for cast
i. Quality of plaster most important (Barton)
ii. Preferred - Plaster of Paris (allows molding into palm); or thin layer of Plaster of Paris (snug and well molded), reinforced with fiberglass
iii. Regular check to maintain snug fit, and rigid immobilization
iii. Expected time to union
1. Distal third 6-8 weeks
2. Middle third 8-12 weeks
3. Proximal third 12-24 weeks
iv. Healing rate and prognosis
1. Tuberosity and distal third - 100 %
2. Waist - 80-90 %
3. Proximal pole - 60-70 %
(Proximal fractures prone to non-union and osteonecrosis; delay in starting immobilization leads to higher rate of non-union (Langhoff & Anderson 1988))
Electrical or ultrasound bone stimulation to promote union has shown encouraging results, with cast immobilization (Divelbiss et al 2001) Radiological features of acute Scaphoid fractures cannot be used to predict likelihood of union (NJ Barton & TRC Davis 1999)
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
v. Current recommendation for management in cast
1. Colles type POP, well molded into palm (use bandage roll)
2. Thumb free
3. Wrist in 20 degree extension
4. Elbow not included unless patient profile demands
5. Follow up weekly to check snug fit and cast integrity
b. Operative treatment
i. Indications:
1. Fracture displacement > 1 mm
2. Trans-Scaphoid peri-lunar dislocation
3. Unstable fractures (Herbert classification)
4. Fractures known for AVN
Proximal pole
Vertical oblique
Comminuted
Diagnosed late (after 4/52)
5. Radiolunate angle > 15 degrees
6. Scapholunate angle > 60 degrees
7. Humpback deformity
8. Non-union
ii. Technique
1. Approach
Percutaneous (94-100 % union rates, and 0-30 % complication rates reported - comparable to open technique - Bushnell et al, 2007)
i. Recommended only for non-displaced or minimally displaced Scaphoid fractures
ii. Volar or dorsal approach
iii. Can be used for displaced fractures with reduction of fracture under fluoroscopic or arthroscopic control
(Requires high level of experience and skill)
iv. Requires high level of experience and skill
v. Dorsal approach complications up to 30% and it is advised now to use mini-open approach
AARIF, arthroscopic assisted reduction and internal fixation of scaphoid fractures (JHS Am Aug, 2001)
i.
Volar approach
i. Through bed of FCR
ii. Good exposure of waist and distal fractures
iii. Procedure (Joe Dias)
1. Landmarks - Scaphoid tubercle & FCR tendon
2. Incision along radial border FCR tendon to Scaphoid tubercle, then angle radially in direction of APB
3. Dissect through bed of FCR tendon sheath
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
4. Incise and reflect capsule, radioscaphoid & radioscapholunate ligaments.
5. Define scaphotrapezoid joint by reflecting scaphotrapezoid ligament radially.
Dorsal approach
i. Between EPL and EDC (extensor compartments III and IV)
ii. Good exposure of proximal fractures (proximal third)
iii. Take care to preserve blood supply to Scaphoid (enters along dorsal ridge)
iv. Procedure
1. Incision - longitudinal over Lister's tubercle
2. Incise extensor retinaculum and compartment IV
3. Reflect ECRB & EPL radially
4. "L" shaped incision of dorsal ligament reflecting flap to the radial side, to access the joint
5. Flex wrist 90 degrees to expose the proximal pole and fracture.
2. Fixation
Herbert screw
Herbert-Whipple screw
AO low profile compression screw
Accutrac screw
K-wires
3. Postoperative immobilization
Initially back slab for 10-14 days then splint until union
If patient unreliable then pop cast for 4-6 weeks iii. Complications
1. Infection
2. Wound complications
3. Injury to nerves (cutaneous branches of radial)
4. Injury to ligaments
5. Injury to tendons
6. Disruption of vascular supply to Scaphoid
7. Instrumentation failure, or removal required
8. Risks of associated anaesthetic technique
|
||
|
|
||
|
10) Sequelae of Scaphoid fractures
a. Delayed union i. > 4 months
b. Malunion
i. Scaphoid may heal in flexed position "Hump back" deformity
|
||
|
|
||
|
|
||
|
|
||
|
|
|||
 |
|||
|
|
|||
|
Development of the dorsal humpback deformity of the Scaphoid after fracture of the Scaphoid waist
Angulation between the proximal and distal Scaphoid fracture fragments
Fragments settle or impact into each other
Bony prominence (the humpback deformity) develops dorsally at the fracture site
CT measurements defining a "Hump back" deformity
i. Intra-scaphoid angle > 45 degrees (Normal = 24 degrees)
ii. Ratio: Scaphoid height / length > 0.64
|
|||
|
|
|||
 |
CT view (Long axis
|
||
|
|
|||
|
Scaphoid) depicting "Hump" back deformity
|
|||
|
|
|||
|
c. Avascular necrosis
|
|||
|
|
|||
|
|
|||
|
|
|||
|
|
|||
 |
X-ray PA showing AVN
|
||
|
|
|||
|
d. DISI (Dorsal intercalated segmental instability [DISI])
i. Lunate and Triquetrum assume a position of excessive dorsiflexion with Scaphoid fractures
ii. Scapholunate angle > 70 degrees
|
|||
|
|
|||
 |
|||
|
|
|||
|
e. Non-union
i. No union beyond 6 months
ii. Longer duration of non-union - worse prognosis for successful management
iii. Contributing factors
1. Inadequate immobilization
2. Insufficient period of immobilization
3. Severe displacement of fracture fragments
4. Associated carpal instability
5. Treatment failure
iv. Natural history
1. Persistent pain (not always present)
2. Progression of arthritic changes (5-20 years)
3. Displacement of non-united fragments with incongruency and carpal instability
4. Scaphoid non-union advanced collapse (SNAC)
v. Clinically
1. Vague wrist pain
|
|||
|
|
|||
|
|
|||
|
|
|||
|
|
||
|
2. Decreased range of motion - wrist joint
vi. Imaging
1. X-ray
Proximal pole AVN
May indicate non-union
2. CT
Shows cortical bridging (Degree and position of non-union)
Intra-Scaphoid angle
Height / length ratio
3. MRI
Assess vascularity
vii. Management
1. Better prognostic factors:
< 40 years of age
Non-union < 2 years
No AVN
No malalignment
Proximal pole not involved
Can even consider attempted conservative measures (69 % union) -cast up to 6/12; electromagnetic- or ultrasound stimulation - mostly restricted to patients with contra-indication for surgery
2. Poorer prognosis expected:
Non-union more then 5 years
Proximal pole non-union
Malalignment
AVN
Manual labourer
Requires surgery
3. Options for surgical treatment of non-unions in absence of OA
Non-vascularized bone grafting i. Matti-Russe
1. Cancellous bone graft (Iliac crest) into cavity created within fracture fragments @ site of non-union
2. Union rates of approximately 90 % (failed cases due to AVN of proximal pole)
3. Difficult to correct "Hump back" deformity
1. Done with intercalated wedge bone graft, fixed with K-wires (77 % union) or screw (94 % union) (Merrel et al 2002)
2. Stark et al, 1988; suggested correction of "Hump back" deformity through forceful extension, followed by transfixing fragments with K-wires (in correct position), cancellous chips then tightly packed into void (97 % union rate reported, and less challenging then wedge graft)
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
3. Finsen et al, 2006; supported Stark et al and also reported excellent results for proximal pole non-unions 4. Limited data on proximal pole fractures with AVN, but union rates reported 40-67 % with non-vascularized grafting (Krimmer 2002) ii. Revision surgery after failure of non-vascularized graft likely to be unsuccessful (Merrel et al 2002)
|
||
|
|
||
 |
||
|
|
||
|
Matti-Russe non-vascularized graft
|
||
|
|
||
|
Vascularized bone grafting
i. Advantages
1. Potentially more reliable union (advantage)
2. Preservation of blood supply
3. Primary bone healing
ii. Should be considered in case of:
1. AVN
2. Proximal pole non-union
iii. Poor candidates for vascularized graft include
1. Those with carpal collapse
2. Large defect in Scaphoid
3. Extensive comminution
4. Radiocarpal arthritis
iv. Methods
1. Kawai and Yamamoto
1. Pronator quadratus pedicled bone graft
2. Volar approach
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
3. Short arc of rotation
4. Tenuous blood supply
5. Palmar radiocarpal ligament dissection
2. Pedicled grafts based on ulnar- or palmar carpal artery
3. Radial styloid fasciosteal graft
4. Pedicled grafts from 1st or 2nd metacarpals
5. Free vascularized bone grafts from iliac crest and medial femoral supracondylar region have also been reported
6. Zaidemberg (1,2 ICSRA)
1. Dorsal approach (Proximal pole)
2. Vascularized bone graft derived from dorsal radial aspect of distal radius nourished by1,2 intercompartmental supraretinacular artery
3. Recent papers on vascularized bone grafts mostly utilize this method
7. Shin et al, 2004; Mayo clinic (N=52)
1. 1,2 ICRSA utilized
2. 72 % overall union (average 16 weeks)
3. Factors adversely affecting union:
i. Female (30 % vs. 82 % in males)
ii. Smoker (46 % vs. 81 % in non-smokers)
iii. Proximal pole AVN (48 % vs. 91 % in absence of AVN)
iv. Type of fixation (53 % union with K-wire fixation vs. 88 % utilizing screw fixation)
v. "Hump back" deformity present in 50 % of failures vs. 11 % of patients who went on to union
vi. 64 % healing rate in patients with prior surgery compared to 73 % in those with no previous surgery
4. Union rate 100 % in patients with no AVN and screw fixation
Outcome
i. 25 % failure rate
ii. Persistent pain and stiffness
iii. Proximal pole necrosis 46 %
iv. Radiocarpal arthritis 54 %
v. Patients worse after failed surgery
f. Non-union with OA (SNAC) - often equates to salvage procedure
i. Sequence of events
1. Scaphoid non-union advanced collapse
2. Carpus shortens
3. DISI
4. Arthritis
ii. Arthritis progression
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
1. Stage I: Arthritis localized to the distal Scaphoid and radial styloid
2. Stage II: Arthritis affecting entire radioscaphoid joint.
3. Stage III: Arthritis affecting the entire radioscaphoid joint, and the capitolunate articulation
4. Stage IV: Radiocarpal joint and intercarpal joints are affected, and may involve DRUJ
|
||
|
|
||
 |
||
|
|
||
|
iii. Classification
1. SNAC I - Radioscaphoid OA
2. SNAC II - Radioscaphoid + scaphocapitate OA
3. SNAC III - Radioscaphoid + scaphocapitate + lunocapitate OA
iv. Diagnosis
1. Meticulous physical examination (identify pain generator)
2. Palpating individual joints
Radiocarpal-
Ulnocarpal-
DRUJ
Intercarpal joints
Degeneration within a row, or between rows
3. Prognostic anaesthetic - and or cortisone injections may be helpful
4. Remember to exclude carpometacarpal arthritis as cause for pain (esp. thumb)
5. Meticulous examination of radiographs (PA and lateral usually sufficient)
6. MRI / scintigraphy can be of help (rarely needed)
v. Treatment
1. Non-surgical means
Splint - or cast immobilization
NSAIDs
Selective intra-articular injections of corticosteroids
May provide relief and improved function, but usually of limited or temporary value in more advanced disease (established SNAC)
2. Surgical intervention - Wrist OA
Debilitating pain referable to an osteoarthritic joint
Goal is pain relief and motion preservation in adjacent undamaged joints (as much as possible)
Approach
i. Longitudinal incision in line with third metacarpal to distal radius
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
1. Used in Scaphoid excision, four corner fusion, proximal row carpectomy, total arthrodesis, wrist arthroplasty
2. Incision through skin and subcutaneous tissue to dorsal retinacular structures
3. Third dorsal compartment opened and EPL tendon transposed radially
4. Lister's tubercle exposed (can be removed and used for bone graft)
5. Subcapsular dissection in floor of third compartment extending distally to third metacarpal
6. Alternative capsular incisions
1. Transverse incision for limited arthrodesis
2. Dorsal T-incision for more extensive arthrodesis or proximal row carpectomy
3. Ligament sparing radial-based 7-flap along fibres of dorsal intercarpal ligament (transverse) and dorsal radiocarpal ligament (longitudinal oblique)
7. Note that the posterior interosseous nerve resides on the floor of the fourth dorsal compartment - often resected as part of denervation pain control
ii. Transverse skin incisions are useful in limited arthrodesis, with lesser exposure of localized arthritis
1. Excellent cosmetic result
2. Difficult to extend if needed
3. Risk of nerve injury
iii. Principles
1. Precise incisions with preservation of capsule to allow repair
2. Preserve ligaments (intrinsic and extrinsic) that are not affected by procedure - prevent secondary instability
3. Motion preserving procedures require transverse or ligament sparing capsular incisions
4. Protect fibres of radial and ulnar nerves during exposure
5. Excise posterior interosseous nerve in floor of fourth compartment to aid with denervation
6. With extended longitudinal exposure (total wrist arthrodesis) leave EPL tendon transposed
iv. Use good quality autogenous bone graft
1. Distal radius
2. Proximal ulna
3. Iliac crest
4. Excised carpals generally yields poor quality bone
v. Fluoroscopic examination during surgery
1. Ensure hardware placement
2. Osseous alignment Limited wrist arthrodesis
i. Principles
1. Leave small portion of volar joint intact to preserve carpal spacing
|
||
|
|
||
|
|
||
|
|
||
|
|
||
|
2. Denude osteoarthritic surfaces through hard subchondral bone -more predictable fusion surfaces
3. Use quality autograft (cancellous)
4. Rigid fixation to allow early range of motion and prevent stiffness
5. Check hardware placement (fluoroscopy)
6. Ensure alignment corrected with fluoroscopy prior to fixation
1. DISI - lunate needs to be brought out of extended position (K-wire joystick)
7. Serial postoperative x-ray to check on successful fusion
ii. Modes of fixation
1. K-wires
1. Easy to use
2. Reliable
3. Disadvantages
i. Requires POP immobilization
ii. Pin removal
iii. Pin protrusion (infection)
iv. Sensory nerve irritation
2. Standard staples
1. Limited compression
2. Good stability
3. Newer staples provide compression element
4. May impinge with wrist extension
3. Screws
1. Extremely stable compression
2. Headless screws buried
3. Optimal placement can be difficult
4. Dorsal circular plates
1. Minimize impingement
2. Rigid fixation
3. Circumferential compression (theoretically)
4. High non-union and complication rates reported (Vance et al, Kendall et al - Scaphoid graft used)
iii. Scaphotrapezium-trapezoid arthrodesis (STT)
1. STT joint common site of OA (elderly women)
2. Limited dorsal transverse incision and capsular transverse incision
3. Use for treatment of Scaphoid rotary subluxation (SLAC wrist) -controversial
4. Radial styloidectomy always performed with STT arthrodesis to allow maximum motion after fusion (Watson & Ryu, Siegel et al)
5. Care should be taken not to harm volar radiocarpal ligaments
6. On average 65 % of normal wrist motion expected after STT fusion
iv. Scaphocapitate arthrodesis
1. Used for ligament instability involving scapholunate joint
|
||
|
|
||
|
|
||
|
|
||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
2. Same functional outcome as STT fusion, maintaining relative extended position of Saphead, allowing reduction of scapholunate interval
3. Rarely used for treatment of OA
v. Four corner fusion (capitate-lunate-hamate-triquetrum)
1. Radiolunate joint is typically preserved in SNAC / SLAC wrist (four corner fusion contra-indicated in presence of radiolunate arthritis)
2. Reconstruction involves
1. Complete excision of the Scaphoid (care taken to preserve long radiolunate ligament - prevents ulnar translation of the carpal mass)
2. Arthrodesis of Capitate, Lunate, Hamate and Triquetrum
3. Longitudinal skin incision with transverse or ligament sparing capsular incision
4. Fully reduce DISI deformity with temporary K-wire fixation
5. Definite fixation with K-wires / Headless screws or Circular plate
6. Quality bone graft emphasised
7. Expect 75-80 % grip strength and 40-60 % normal motion after four corner fusion
Proximal row carpectomy
i. Excellent salvage procedure - wrist with considerable radiocarpal arthritis
ii. Provided Capitate has no degenerative changes
iii. Transverse or longitudinal incision
iv. Bones of proximal row are removed either side of tendons of fourth dorsal compartment
v. Extreme care to preserve radioscaphocapitate ligament (prevents ulnar translation of Capitate of distal radius
vi. After removal of Scaphoid, Lunate and Triquetrum, distal row migrates proximally
vii. Head of Capitate articulates with lunate fossa of the distal radius
viii. Excellent results reported by multiple authors
ix. 80 % of normal grip strength, and 60 % of normal motion
x. Secondary degenerative changes may eventually be seen at radiocapitate articulation over time (greater risk in young active patients)
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
|
||||||||||||||||||||||
|
Distal Scaphoidectomy
i. Excision of distal pole of scaphoid
1. Concerns about promoting instability
2. Intact scapholunar ligament required
3. May be efficacious in treatment of recalcitrant Scaphoid nonunion with concomitant arthritis
4. Ruch & Papadonikolakis (2006)
1. Distal Scaphoidectomy in patients with Scaphoid nonunion after prior surgical treatment
2. Showed improved mean wrist flexion and extension (23 degrees and 29 degrees respectively)
3. Dramatic decrease in pain
4. Average increase in capitolunate angle of only 2 degrees following surgery
5. Concluded distal scaphoidectomy a valuable option in treatment of patients with failed prior surgical attempts at Scaphoid union
Total wrist arthrodesis
i. Standard surgical treatment for pancarpal degenerative joint disease in patients who wish to undertake considerable heavy labour
ii. Good function after surgery
1. Strong grip (some extension of wrist required in arthrodesis alignment(10-15 degrees))
2. Predictably excellent results in 93-100% (Weis et al, Hastings et al)
iii. Pain relief less predictable (O'Bierne et al, Sagerman et al)
iv. Trouble with
1. Personal hygiene
2. Working in confined spaces
v. Distal radius graft usually sufficient
vi. Precontoured dorsal plates decrease need for long term post operative immobilization
vii. Complicated by
1. Missed DRUJ arthritis
2. Ulnocarpal impaction
Total wrist arthroplasty (TWA)
i. ADL made easier with some wrist motion
ii. TWA more attractive in low demand individuals with pancarpal osteoarthritis
iii. Initial TWA by Swanson (Silicone)
1. Good pain relief
|
||||||||||||||||||||||
|
|
||||||||||||||||||||||
|
|
||||||||||||||||||||||
|
|
||||||||||||||||||||||
|
|
||
|
2. High implant failure
3. Reactive synovitis with secondary osteolysis iv. New generation TWA
1. Articulated
2. Enhanced arc of motion (some problems with stability)
3. Shown to predictably provide pain relief (most data from RA patients)
4. Maintains 60 degrees arc ROM split between flexion and extension
5. Postoperative activity restrictions
1. Avoid impact loading
2. Avoid lifting > 10 lb
6. Low demand patients Wrist denervation
i. Introduced by Wilhelm 1958
ii. Initially described utilizing five separate incisions
iii. Modality for treatment of chronic wrist pain often in conjunction with partial arthrodesis
iv. Deneravation of sensory supply to wrist
1. Palmar aspect
1. Anterior interosseous nerve
2. Palmar cutaneous branch of median
3. Lateral antebrachial cutaneous
|
||
|
|
||
 |
||
|
|
||
|
2. Dorsal aspect
4. Posterior interosseous nerve
5. Dorsal branch of ulnar nerve
6. Superficial branch of radial nerve
|
||
|
|
||
|
|
||
|
|
||
|
|
||

|
||
|
|
||
|
v. Current authors (Gerrit et al 2006)
1. Two incisions (one palmar and one dorsal)
2. Possible to disconnect periosteum from capsule & interrupt majority of capsular nerve fibres
|
||
|
|
||
|
|
||
|
|
||