Internal Rotational Deformities of the
Lower Limb
Jason Crane
May 2008
Abstract
Most rotational variations in young children, such as in-toeing, out-toeing, and torticollis, are benign and resolve spontaneously. Understanding the normal variations in otherwise healthy children is vital to identifying true structural abnormalities that require intervention. A deliberate assessment of the rotational profile is necessary
when evaluating children who in-toe or out-toe. In-toeing is usually attributable to metatarsus adductus in the infant, internal tibial torsion in the toddler, and femoral anteversion in children younger than 10 years.
Definition
Rotational profiles vary widely among normal children. Differences in appearance during walking or running are most often just that, differences and not pathological conditions. In toeing is described by the direction of the foot, relative to the body’s line of progression during the gait cycle. This is referred to as internal torsion. It is produced by the summation of factors that include version of the bones, capsular laxity or tightness and muscle control.
Natural History
Limb buds appear in the fifth week in utero. The great toes develop in a preaxial position, rotating medially in the seventh week to bring the hallux to midline. Subsequent intrauterine molding causes external rotation at the hip, internal rotation of the tibia, and variable positioning of the foot. Thus, many infants are born with an internal tibial torsion axis, an external contracture at the hip, or flexible foot deformities.
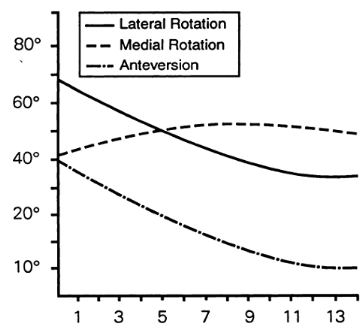
The external hip contracture initially masks the high degree of femoral anteversion also characteristic of normal infants at birth. Postnatally, the lower extremities continue to rotate externally until adult values are reached (between ages 8 and 10 years). During this period of rapid growth, the tibia typically externally rotates 15° (-50 at birth to10o at maturity) while femoral anteversion decreases an average of 25° (400 at birth to 15o at maturity). Normal rotational profiles in childhood therefore are variable and age-dependent.
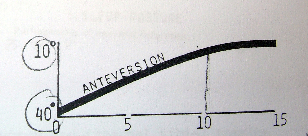
Femoral anteversion progression with age Tibial rotation progression with age
Evaluation
Normal variability in young children must be differentiated from more serious structural problems. The clinical history should delineate the onset and duration of a structural problem and any evidence of progression. Whereas the typical natural history of benign rotational conditions would suggest improvement over time, a progressive deformity suggests a possible pathologic developmental or neurologic disorder.
history should include a careful assessment of rotational disorders in other family members and the presence of hereditary disorders (eg, vitamin D–resistant rickets, mucopolysaccharidoses, achondroplasia, epiphyseal or metaphyseal dysplasia) that may affect the rotational profile.
The child’s rotational profile, as described by Staheli, should be recorded.
The five components in this profile are:
Internal and external hip rotation, Thigh-foot axis, Transmalleolar axis, Heel-bisector angle, Foot progression angle during gait.
Internal and external hip rotation.
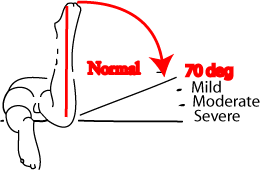
Hip rotation is most easily measured with the patient in the prone position. Infants have an average of 40° of internal rotation (range, 10° to 60°. The range is limited by the tight posterior capsule even though they have increased femoral anteversion and should potentially have a larger internal rotation arc.) and 70° of external rotation (range, 45° to 90°). By age 10 years, internal hip rotation averages 50° (range, 25° to 65°) and external rotation, 45° (range, 25° to 65°). Internal rotation measuring 70°, 80°, or 90° is evidence respectively of a mild, moderate, or severe increase in femoral torsion. Increased femoral torsion may be evident during gait, with medially facing patellar alignment.
![[image]](internal-rotational-deformities-of-the-lower-limb/internal-rotational-deformities-of-the-lower-limb-3.png)
Thigh-foot axis
Is best examined with the child in the prone position and the knee flexed 90°. This angle consists of the rotation of the tibia and hindfoot in relation to the longitudinal axis of the thigh and indicates the amount of tibial torsion present. In infants, the thigh-foot angle averages 5° internal (range, 30° to +20°). Excessive internal tibial torsion spontaneously resolves by age 3 or 4 years in most children. By age 8 years, the thigh-foot axis averages 10° external (range, 5° to +30°) and usually changes very little after that.
![[image]](internal-rotational-deformities-of-the-lower-limb/internal-rotational-deformities-of-the-lower-limb-5.png)
Transmalleolar axis
Aids in determining the amount of tibial torsion present. This axis is the angle formed at the intersection of an imaginary line from the lateral to the medial malleolus, and a second line from the lateral to the medial femoral condyles. At gestational age 5 months, the fetus has approximately 20° of internal tibial torsion. The tibia then rotates externally, and most newborns have an average of 4° of internal tibial torsion. As a child grows, the tibia continues to rotate externally. Adults have an average of 23° of external tibial torsion (range, 0° to 40°).
The heel-bisector angle
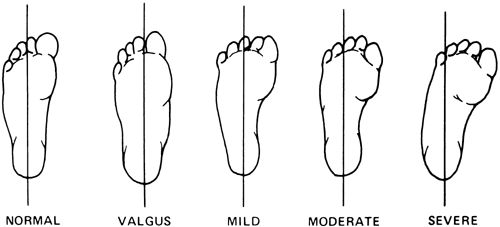
This is the line drawn through the midline axis of the hindfoot and the forefoot. It is helpful in evaluating forefoot adduction and abduction. In a neutral foot, the heel-bisector line passes through the second web space.
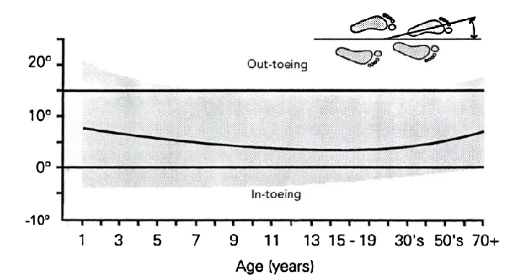
Foot progression angle
The foot progression angle is the angle of the foot relative to an imaginary straight line in the patient’s path. Patients who in-toe are assigned a negative angular value; patients who out-toe are given a positive value. This value represents the sum total
effect of the child’s structural alignment (i.e., femoral torsion, tibial torsion, foot contour) as well as any dynamic torsion forces resulting from muscle forces
Differential Diagnosis
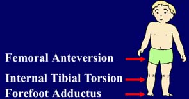
In-toeing usually is caused by benign conditions such as metatarsus adductus, excessive internal tibial torsion, and excessive femoral torsion. Less frequently, patients have pathologic conditions such as clubfoot, skewfoot, hip disorders, and neuromuscular diseases. Metatarsus adductus, with or without internal tibial torsion, is the most common cause of in-toeing from birth to 1 year. In toddlers, internal tibial torsion causes most in-toeing. After age 3 years, in-toeing usually is caused by increased femoral anteversion. More severe in-toeing suggests a combination of deformities, such as internal tibial torsion and excessive femoral anteversion.
Out-toeing typically is caused by external rotation contracture of the hip, external tibial torsion, or external femoral torsion. External rotation contracture of the hip capsule is a common finding during infancy, whereas external tibial or femoral torsion is more commonly seen in older children and adolescents who outtoe. Severe pes planovalgus also has been associated with out-toeing. More serious conditions, such as a slipped capital femoral epiphysis, hip dysplasia, or coxa vara, are less common but should be considered. Severe Cerebral palsy children may develop femoral internal rotation and tibilal external rotation, called miserable alignment syndrome.
Treatment
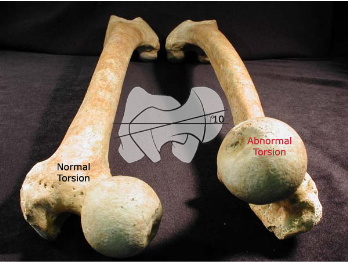
Active treatment of childhood rotational disorders is unnecessary in most cases. Treatment consists of reassurance and education about the natural history of the condition. Bracing and shoe modifications are unnecessary and should be actively discouraged for these normal children.
![[image]](internal-rotational-deformities-of-the-lower-limb/internal-rotational-deformities-of-the-lower-limb-9.png)
Metatarsus Adductus
Definition
Described by Henke in 1863, metatarsus adductus is the most common pediatric foot problem referred to orthopaedic surgeons. It consists of medial deviation of the forefoot on the hindfoot with a neutral or slightly valgus heel.
Incidence
Occurs in 1:5,000 live births and in 1:20 siblings of patients with metatarsus adductus. The rate of metatarsus adductus is higher in males, twin births, and preterm babies.
Pathogenesis
Although the exact cause of metatarsus adductus is unknown, numerous theories exist. One is that in utero positioning causes the deformity. Earlier studies suggested a relationship between metatarsus adductus and hip dysplasia, but recent studies indicate no such correlation.
Clinically
Metatarsus adductus usually is seen in the first year of life and occurs more frequently on the left side. Presenting complaints include cosmesis, an in-toeing gait, or excessive shoe wear. On physical examination, the foot appears C-shaped, with a concave medial border and a convex lateral border. The hindfoot will be neutral or in valgus, but never in varus. Range of motion of the ankle and subtalar joint will be normal.
Classification
Depending on the heel-bisector angle metatarsus adductus has been classified by Smith et al as mild, moderate, or severe. A later classification system described by Bleck designated a flexible forefoot as one that could be abducted beyond the midline heel bisector angle, a partially flexible forefoot as one that could be abducted to midline, and a rigid forefoot as one that could not be abducted to midline.
Radiology
The usefulness of radiographs before age 4 years is limited by the lack of sufficient ossification in the bones of the foot. In older children, forefoot adduction, excessive medial deviation at the tarsal-metatarsal joint, and a neutral or valgus heel will be evident on a standing radiograph.

Management
Conservative
Most cases of flexible metatarsus adductus resolve spontaneously and do not require use of splinting, braces, or special shoes. In a series of 21 patients (31 feet) with partly flexible or inflexible metatarsus adductus treated with serial casting, 20 patients (95% [29 feet]) had painless normal feet as adults Most evidence indicates that flexible metatarsus adductus commonly resolves without treatment and that even when it does not, it rarely leads to pain in adulthood. Patients with rigid metatarsus adductus deformities should undergo early casting.
Surgical
Uncommonly, resistant cases of inflexible metatarsus adductus that do not reduce with serial casting may require surgery because of painful shoe wear. Surgery is planned between three and seven years of age (As the midtarsal bones only ossify after 3 years of age). Surgical options include release of the abductor hallucis tendon, medial midfoot capsulotomy, tarsometatarsal joint capsulotomy and release of the intermetatarsal ligaments, or osteotomy at the metatarsal bases and cuneiforms. An opening wedge osteotomy of the medial cuneiform, combined with a closing wedge osteotomy of the cuboid or osteotomies at the base of the second through fourth metatarsals, has been shown to be safe and effective. Thus, this appears to be the most effective surgical option in patients older than 3 years with persistent rigid metatarsus adductus deformities.
Metatarsus Primus Varus
Metatarsus primus varus is an isolated adducted first metatarsal. In contrast with simple metatarsus adductus, in metatarsus primus varus the lateral border of the foot has a normal alignment, and there is often a deepened vertical skin crease on the medial border of the foot at the tarsometatarsal joint. In general, metatarsus primus varus is a more rigid deformity than simple metatarsus adductus, and early casting is recommended. Persistent deformity in childhood is associated with progressive hallux valgus. Opening medial cuneiform osteotomy has been described for selective use in children with a severe deformity.

Dynamic Hallucis Abductus
Dynamic hallux abductus, otherwise known as the wandering or atavistic toe, also can cause in-toeing. The great toe deviates medially during ambulation while the remainder of the forefoot remains straight. Dynamic hallucis abductus usually presents after a child begins walking and is thought to be caused by an imbalance of the great toe abductor and adductor muscles. Dynamic hallux abductus usually resolves with age and subsequent fine motor coordination development.
Skewfoot
Skewfoot, also called congenital metatarsus varus or serpentine metatarsus adductus, is characterized by adducted metatarsals combined with a valgus deformity of the heel and plantarflexion of the talus. Little is known of the pathogenesis of this disorder. Improper casting of metatarsus adductus or clubfoot deformities may result in a skewfoot because of failure to support the hindfoot while abducting the forefoot in
the cast. However, most cases are thought to be idiopathic. The amount of hindfoot valgus necessary to classify a foot as a true skewfoot rather than as the more common metatarsus adductus is not strictly defined.
Standing radiographs confirm the presence of an adducted forefoot and a valgus hindfoot. The natural history of this deformity is unclear. Although some feet undergo spontaneous correction, others clearly continue to have pain, callosities, and problems with shoe wear. Surgery is indicated for children with a persistently symptomatic foot deformity.
Children are treated after age 6 years with an opening wedge osteotomy of the calcaneus and a medial cuneiform opening osteotomy.
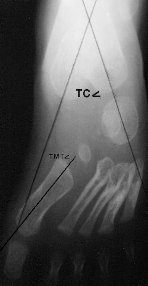
Skewfoot: An AP radiograph reveals the significant varus deformity of the forefoot creating a negatively valued talo-first metatarsal angle. Delayed ossification of the navicular prevents radiographic documentation of the lateral talonavicular subluxation. The hindfoot valgus is portrayed by the increased talocalcaneal angle (the upper limits of normal as shown). Tibial Torsion
Incidence
Internal tibial torsion is the most common cause of in-toeing from ages 1 to 3 years. In two thirds of affected children, the increased torsion is bilateral.
When unilateral, internal tibial torsion usually affects the left side.
Pathogenesis
Most cases are thought to be caused
by intrauterine positioning.
Clinically
Accurate clinical recognition relies on measurement of the thigh-foot and transmalleolar axes. Parents of children with increased internal tibial torsion often report that the child is clumsy and trips frequently.
Treatment
Conservative
Treatment with splinting, shoe modifications, exercises, and braces has proven to be ineffective. Because the natural history of internal tibial torsion strongly favors spontaneous resolution by age 4 years, expectant observation is recommended instead. Disability from persistent residual internal tibial torsion is rare, and it has been found not to be a risk factor for degenerative joint disease. Some have even suggested that in-toeing improves sprinting ability.
Surgical
Surgical treatment of tibial torsion is rarely indicated and should be re- served for children older than 8 years with marked functional or cosmetic deformity and a thigh-foot angle greater than 15°. Both proximal and supramalleolar tibial derotational osteotomies have been used to manage tibial torsion. However, most surgeons prefer the supramalleolar osteotomy because of its lower complication rate. In the skeletally mature adolescent, derotational osteotomy with intramedullary fixation is also an option.
Femoral Torsion
Definition
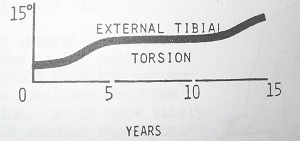
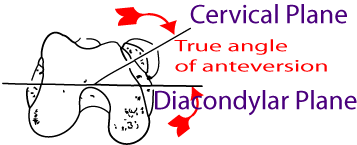
Femoral torsion is the angular difference between the femoral neck axis and the transcondylar axis of the knee.
Development
At birth, neonates have an average of 40° of femoral anteversion. By age 8 years, average anteversion decreases to the typical adult value of 15°.
Pathogenesis
Most cases of femoral torsion are idiopathic, although a familial association is identified in some patients. No association between increased femoral anteversion and degenerative joint disease has been proved; however, some association with knee pain has been suggested. Knee pain may be particularly prevalent in children with concomitantly increased femoral anteversion and external tibial torsion (so-called miserable malalignment syndrome).
Etiology
Increased femoral anteversion is the most common cause of in-toeing in early childhood, tends to occur in females, and is symmetrical.
Clinically
Children with excessive femoral anteversion characteristically sit with their legs in the W position and run with an eggbeater-type motion (because of internal rotation of the thighs during swing phase). In-toeing from excessive femoral anteversion usually increases until age 5 years and then resolves by age 8.

On physical examination, internal hip rotation is increased and external hip rotation decreased (>700 internal rotation is classified as abnormal). Using Craig’s test; Patient lies prone with knee flexed 900 and examiner palpates posterior aspect of greater trochanter. Hip is then passively rotated internally and externally until greater trochanter is parallel with examining table or reaches its most lateral prominent position. The degree of anteversion can then be estimated, based on the lower leg's angle with the vertical.
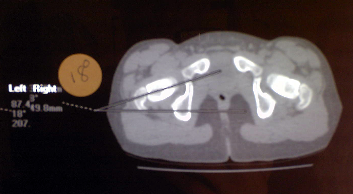
Radiology
Previously plain X-rays using the Magillian method (complicated set of graphs and tables) were utilized to calculate the femoral anteversion. Fluoroscopic methods using a goniometer intra procedure have also been described. These methods have been largely replaced by CT-Scan. Cuts are made through the femoral neck and the femoral condyles with the patient in a static position this gives an accurate representation of the femoral anteversion.

Treatment
Conservative
Femoral anteversion is usually self-limiting, and if persistent causes no long term pathological changes in the associated joints. No treatment is necessary for most cases of femoral torsion.
Surgical
Surgical intervention may be indicated in a child older than 8 years with a marked cosmetic or functional deformity, anteversion >50°, and internal hip rotation >80°. Surgeries to correct femoral torsion include proximal femoral, distal femoral osteotomies and intra medullary nails. Todd etal suggested a proximal femoral osteotomy may be considered if the patient has a concomitant varus or valgus deformity. Otherwise, a distal femoral osteotomy through a lateral approach is the preferred treatment. A small compression plate may be used to treat skeletally immature patients and a blade plate for skeletally mature patients. This is controversial as many authors believe you should correct proximally at the cora of the deformity. They also believe that a distal rotational osteotomy will result in patella maltracking and patellar femoral pain, while others maintain that you are correcting the deformity to its normal anatomical profile and there for no maltracking should occur.
Summary
Benign rotational variations are seen in many healthy children. Although the physical appearance of these conditions may initially be alarming, spontaneous resolution occurs in most cases. A thorough understanding of the normal rotational variations that may occur in children younger than 10 years is essential to properly reassure and educate families, as well as to identify more serious underlying structural problems that might exist.
References
Common Rotational Variations in Children; Todd L. J Am Acad Orthop Surg 2003;11:312-320
Torsional Deformities. Schoenecker PL; AAOS 23rd annual comprehensive review course for orthopaedic surgeons, June 2007
Rotational Problems in Children; Staheli L. J Bone Joint Surg Am. 1993;75:939-949.
Lower-extremity rotational problems in children. Normal values to guide management. LT Staheli, J Bone Joint Surg Am. 1985;67:39-47
|