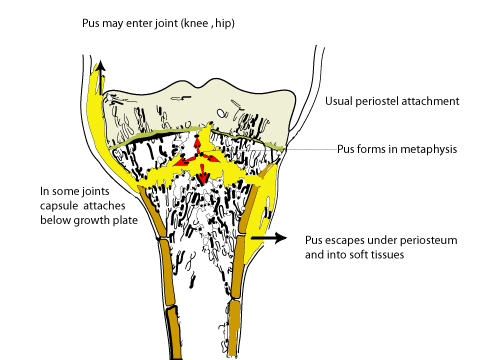
Acute osteomyelitisAcute Osteomyelitis presents with an acute pyrexia illness. The child is toxic and ill and complains of bone pain. In South Africa osteitis is common, and must be suspected in any child who presents with a painful limb together with a pyrexia illness. In a late case the limb may be swollen, with pitting oedema resembling cellulitis. Children seldom develop cellulitis without an underlying cause - consider osteomyelitis in all children with "Cellulitis". Before antibiotics the mortality from this illness we 20-30%, but today fatalities are rare. There is, however much morbidity, especially if the diagnosis is delayed and chronic osteomyelitis develops. PathogenesisThe primary septic focus is often a septic skin lesion such as scabies, a septic tooth or other lesion. The child is often undernourished and the disease is often associated with poverty. There may be a history of minor trauma, the organisms seed to the metaphysis and form a small abscess, perhaps in the pre-existing haematoma. The pus builds up in the metaphysis and later escapes under the periosteum.
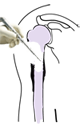
By this time there is a general septicemia and the child is toxically ill. In some areas such as the hip and knee the metaphysis is partially intra capsular and escape of this pus can cause a septic arthritis to complicate the original osteomyelitis. The growth plate acts as a barrier and the pus cannot cross it directly into the joint. Acute Osteomyelitis is a disease of children. In adults only the vertebrae can be infected. In children all long bones can be affected especially the proximal femur and about the knee. The pelvis and vertebrae are also often affected in children. The septicemia can seed organisms to other bones and other systemic complications such as meningitis, bronchopneumonia and pericarditis are common. The child may present primarily to the paediatric casualty with these complaints and the bone infection can be overlooked.
The causative organism in 95% of cases is Staphylococcus aureus. Haemophyllis influenza is common under 2 years of age. In the immune suppressed, virtually any organism can be the cause.
ClinicalBy the time most children present to casualty they are ill and dehydrated. There is bone pain and tenderness. Percussion over a bony prominence near the infected area produces acute pain. Remember to examine the child thoroughly for other areas of osteomyelitis as well s to move the joints for sighs of septic arthritis. If the child has been on oral antibiotics the above signs may be masked and the diagnosis is thus more difficult. Check the neck for signs of meningism. Listen to the lungs and heart for signs of pneumonia or a pericardial friction rub.
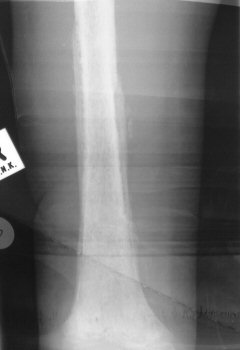
Special InvestigationsThe white cell count and ESR are raised. Take blood for a blood culture - positive in 80%. A Technetium scan will be positive, but is time consuming and is not usually necessary as the diagnosis can be made without it. There is more urgency to get the child to theater and drain the bone. X Rays are normal, except for possible soft tissue swelling. Check for effusions in adjacent joints - this may denote septic arthritis or a sympathetic effusion secondary to the inflammation caused by the osteitis. After about 10 days signs such as a periosteal reaction will appear. If treatment does not abort progress of the infection, signs of chronic osteitis such as invulucrum and sequestrum will become visible on x ray. Technetium bone scans may be useful if there is doubt about the diagnosis. A false negative bone scan may be seen in up to half the cases.
TreatmentThe child is often dehydrated. Insert an intravenous catheter and re hydrate, at the same time blood can be taken for culture, full blood count and ESR. The aim is to resuscitate the patient and get her to theater for drainage as soon as possible. In South Africa most cases present late (2 to 3 days after onset) and because of this operative treatment is mandatory. If other medical conditions, such as bronchopneumonia, meningitis etc complicate the osteitis these will need attention too. Drainage of the pus is an emergency procedure and should not be delayed unnecessary because of the need for bone scans and other non essential investigations. If on clinical grounds the site of the lesion can be localized, proceed with the drainage operation. If the site cannot be localized a technetium scan is invaluable. In theater the site is approached via an appropriate operative approach. Go for the metaphysis, even if the skin is swollen over the diaphysis, the pus originates in the metaphysis and this must be drained. Drill 2 or 3 small holes in the cortex over the metaphysis. In an early case pus will stream out of the bone. In a advanced case the pus has already escaped and may have to drained subperiosteally along the whole shaft. Break down any loculi so that the pus can drain freely. Resist the temptation to drain the diaphysis even if there is pus along it. This creates a stress raiser which may lead to a septic pathological fracture. If much pus was encountered, leave the wound open for secondary suture later - a "second look" operation is advised 24 to 48 hours later if the temperature does not resolve and the wound remains contaminated. take numerous pus swabs for microscopy and sensitivity studies. Intravenous antibiotics are begun. If an appreciable delay is anticipated before theater, these may be started preoperatively, but they may mask bacteriological analysis of the pus. Because the type of organism will not be known until later, begin with an antibiotic effective against S. aureus such as Cloxacillin (100 mg /kg intravenously followed by 200mg /kg/day, divided into six-hourly doses) and supplement it with something that will kill H. influensae such as Erythromycin. Fucidic acid and Erythromycin is also effective as is a first generation cephalosporin. By day 3 the sensitivity will be known and the antibiotics can be changed if necessary. The pyrexia should abate by day 2 postop. If it persists the cause may be the same site that was incompletely drained, another bone or joint becoming infected, of a non skeletal source such as bronchopneumonia.
Postoperative physiotherapy is given to mobilize adjacent joints. The limb may need protection by means of a back slab, splint or traction (hip region). The Erythrocyte sedimtation rate (ESR) should fall in the ensuing weeks. If it does not, the patient may be developing chronic osteomyelitis. Antibiotics are continued intravenously while the child is pyrexial. Once the temperature abates an oral form of the antibiotic can be given. Continue for a minimum of three weeks with antibiotics. If X rays and a high ESR show the osteomyelitis is becoming chronic, it may be necessary to continue longer. Once sequestrae are seen antibiotics will be ineffective and surgical measures such as a sequestrectomy may be considered.
After discharge from hospital the weakened bone may need protection by a cast or use of crutches. Before involucrum has formed the osteopaenic bone can fracture easily. A fracture through a septic bone is difficult to treat.
Chronic OsteomyelitisEstablished osteomyelitis consists of new bone formation - the involucrum. Dead bone- known as sequestrum acts as a nidus of infection. Antibiotics will be ineffective until this is removed.
Sequestrectomy operationIt is important to improve the host condition. Immune suppressing diseases are usually the reason for persistence of chronic osteomyelitis. Comorbid conditions, such as diabetes and HIV/ AIDs must be brought under optimal control before any surgery is undertaken.
Complications
|
Acute Osteomyelitis
Department of Orthopaedic Surgery - Stellenbosch University
| Acute and Chronic Osteomyelitis |