Clinical education overview
What is clinical education?
Placing students in the clinical environment allows them the opportunity to practice what they have learned in the classroom in real-life situations, as well as develop professional skills that cannot be taught in the classroom. Clinical education is offered under the supervision of qualified clinicians and / or faculty staff.
the workplace is where the professional learning is made real, where knowledge and skills are acquired, crafted and developed." Morris and Blaney, 2014

How students learn

To facilitate good clinical learning we need to first consider how students learn in the clinical context.
What are some learning theories applicable to clinical education?
Learning theories
Presented below is an overview of several learning theories.
A tool to understanding how learning develops in increasing complexity.
The clinical setting is where the student will have the opportunity to move from knowledge and understanding, towards applying and analysing. In the 4th year of clinical exposure, the student is then facilitated towards the upper most levels of evaluating and creating.
#TIP: Do not assume the knowledge and understanding is established. Probe first to establish the level of knowledge and understanding and any gaps, before expecting application and analysis. Encourage the student to revise prior taught knowledge. Understand that engagement in the higher, more complex levels can only happen when the foundation levels are in place.
Scaffolding for learning is understanding that the student may need to master smaller, more manageable tasks first, before reaching the ultimate learning goal. Scaffolding supports student learning towards increasing levels of independence
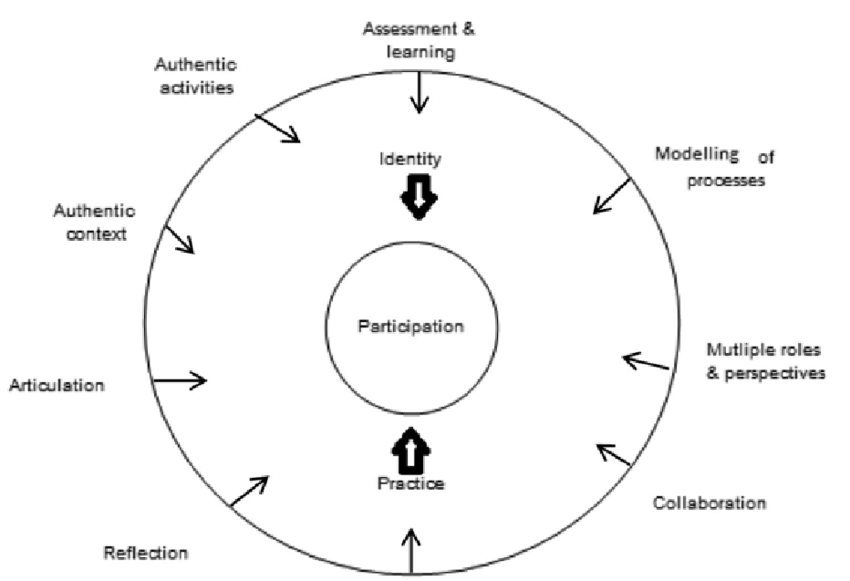
Situated learning theory proposes that students learn within a community of practice (COP), moving into fuller participation through various learning activities. As educators and clinicians, we form part of that COP providing the support and facilitation to students to developing their professional identity and independence.
” New learners enter the COP at the edge of the community and learn through a process of legitimate peripheral participation in which they observe and perform less vital tasks of the community. As they take on more responsibility in the community, learners move towards the centre……and come to understand the particular knowledge that distinguishes that community from others.” Kauffman and Mann, 2014
Social learning theory, proposed by Albert Bandura, emphasizes the importance of observing, modelling, and imitating the behaviors, attitudes, and emotional reactions of others.
Role modelling forms part of social learning theory and can be a powerful tool of learning in the clinical setting. Students learn through the observation of what we as educators do, even when we are not engaged in formal teaching and learning activities with them
#TIPS to using role modelling as an effective learning tool:
- Silent modelling is inadequate as a strategy for teaching (however, be aware that students will be observing ALL you do even when you are not aware).
- The role model’s values, behaviour and justifications must be made clear. Make role modelling explicit.
- Limit the number of possible interpretations to the observed behaviour(s). Do not assume that the student has understood the observed behaviour correctly. Probe for their understanding or interpretation of what they have observed.
- Be gatekeepers to the profession i.e. role model upstanding professional behaviour at all times, with both the patient and all members of the MDT.
Doctor Role Modelling in medicine – BEME Guide No.27
Role modelling—making the most of a powerful teaching strategy
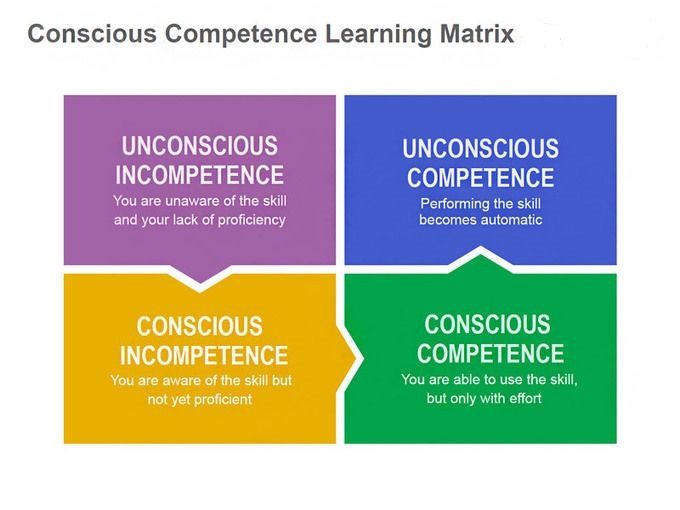
Becoming competent in a skill takes time and practice and moves through a cycle of learning.
Using the table above, consider the example of learning to drive. As a teenager being driven around by your parents, driving looked easy and you may even have been critical of your parents’ driving skill. You did not at that stage understand the complexity of the skill. You were in the unconscious incompetence phase– you did not know what you did not know. Once you obtained your learner’s licence and started to drive you quickly moved into the conscious incompetence phase – you now realised how difficult driving is and became aware of what you did not know. With practice you eventually moved into the conscious competence phase – driving was becoming easier but still requiring effort and concentration. As an adult driving for many years, you now find yourself in the unconscious competence phase – driving a car is easy and requires little effort. It is almost ‘automatic’. However, should you decide to learn to drive a bus, you may find yourself at the beginning of the cycle again.
Applying this to clinical education, sometimes the student is not even aware of what they do not know. Through facilitation we can make them aware of what they do not know and then allow them the opportunity to practice the new skill. With practice they may eventually become competent and be able to do the skill with little effort or thought. Providing adequate feedback between phases helps facilitate the development of the skill.
Transformative learning (TL) has been described as learning that challenges established perspectives, leading to new ways of being in the world”. Van Schalkwyk et al., 2019
Click here to access the full article: Transformative learning as pedagogy for the health professions: a scoping review
Click here to watch a short video outlining Transformative learning
Clinical reasoning
Once we understand how students learn, we can start to apply this knowledge to teaching strategies within clinical education.
An important skill / competency to be facilitated and learned within clinical practice is that of clinical reasoning. A term used often by many a health professional but a term that is perhaps not well understood, especially the learning thereof.
So what is clinical reasoning?
Clinical reasoning can be defined as a complex, cognitive process of making clinical decisions in professional practice (Higgs & Jones, 2008).
The most common model for reasoning clinically is the hypothetical-deductive-reasoning model, outlined in the diagram below. Once all information / data has been collected from the patient, a hypothesis is generated as to the clinical decision to be made. This hypothesis may lead to the need for further data collection. The hypothesis is then tested / validated as being correct or not.
This will eventually lead to a final decision.
Research does however show that experts (those that have practiced for many years) reason clinically through a process of pattern recognition, immediately being able to recognise that which they have seen many times before.
How do we then teach / facilitate clinical reasoning in the student?
- Firstly we need to understand where the student is at in their stage of learning.
- Secondly, it is important to recognise that when starting off in the clinical setting students will often demonstrate a very immature style of clinical reasoning known as 'trial and error'. They lack a hypothesis and are therefore just trying a variety of interventions in the hope that they may be correct.
- Facilitate, therefore, the development of a hypothesis, probing the student for information that they have gathered from the patient's medical records and investigations and their own evaluation of the patient. More often than not the starting point of an incorrect hypothesis is the lack of adequate and thorough data collection from the patient.
- The student can then be guided in testing the hypothesis and then critically evaluating the result. Reflection in action and reflection on action is key to this process. Encourage the student to reflect .
Teaching strategies
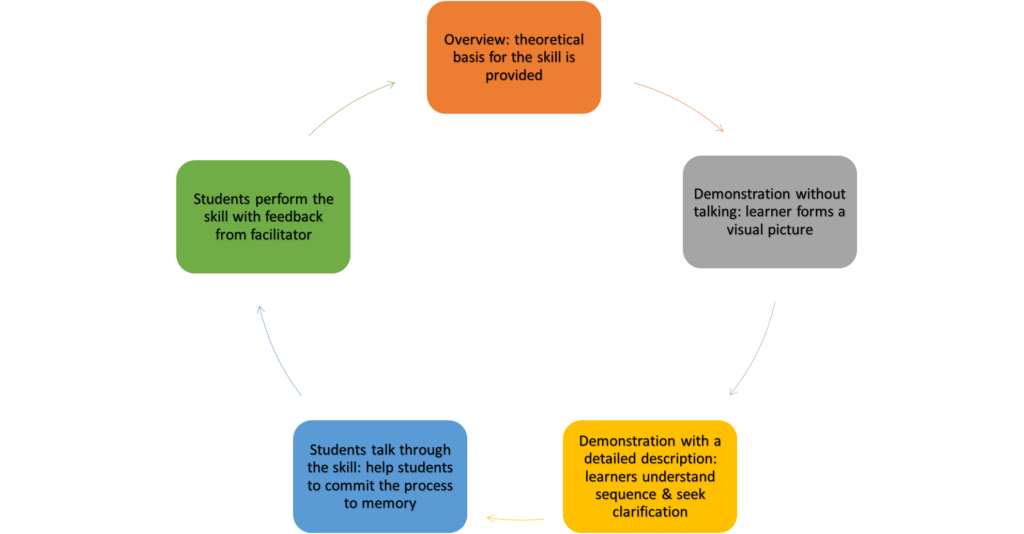
The 5-step method for teaching clinical skills:
Now that we have an overview of some of the theories supporting how students learn we can move towards considering some useful strategies for enhancing teaching in the clinical setting.
The SNAPPS tool is a learner-centered tool that helps students to verbalise their clinical reasoning and ask the ‘right’ questions. The educator takes on the role of a facilitator by promoting critical thinking and in so doing empowering the learner towards their own learning and problem solving capacity.
Feedback and Reflection
here we provides some insight into understanding how students develop their clinical competency through engaging with effective feedback and developing the practice of reflection

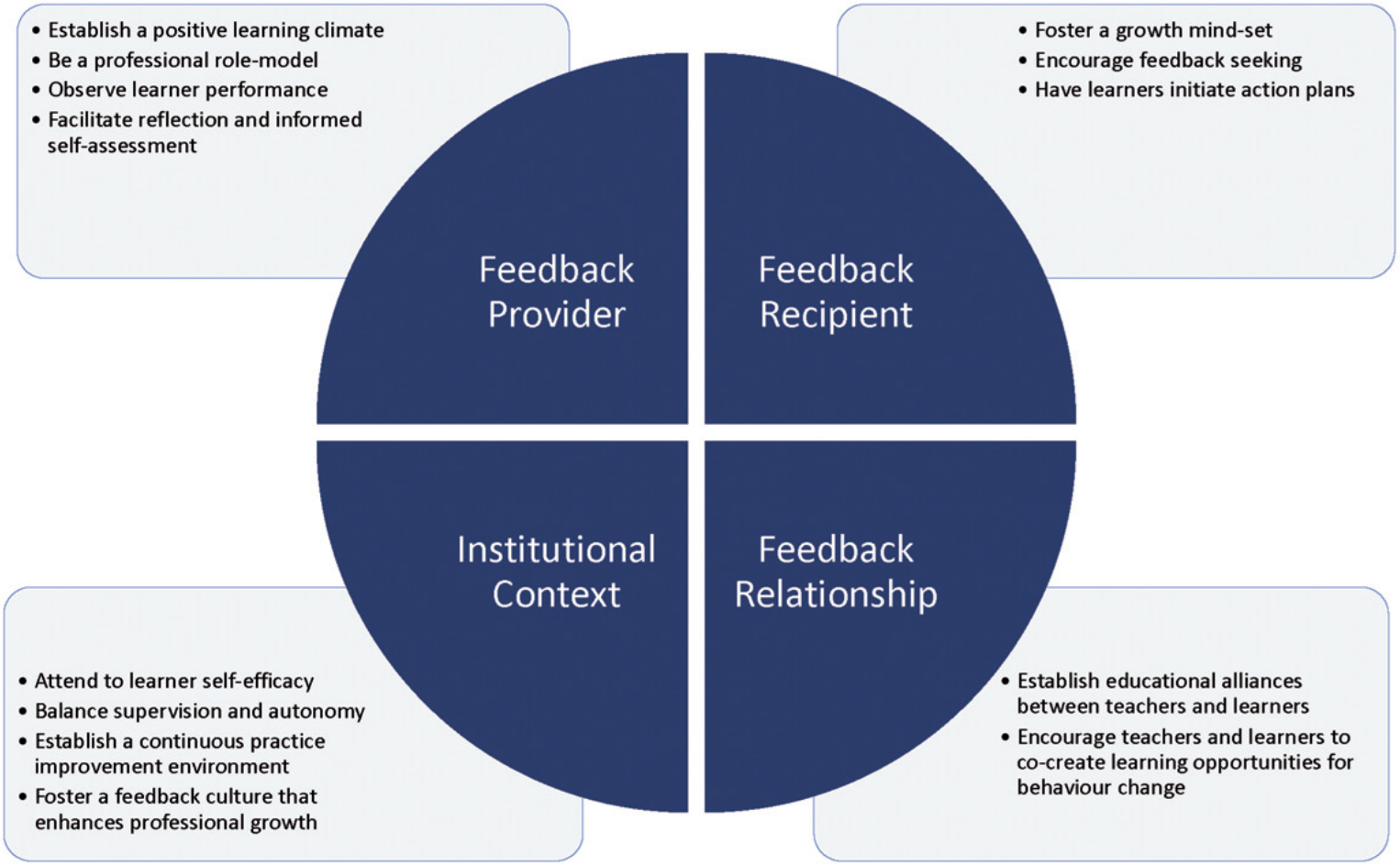
It should be a process in which learners seek to find out more about the similarities and differences between their performance and the target performance, so that they can improve their work. Effective feedback will ensure the closure of a feedback loop, that is, that there is evidence in the student of the feedback having been applied to future practice.
In their article ‘Twelve tips to promote a feedback culture with a growth mind-set: Swinging the feedback pendulum from recipes to relationships’ (Ramani, Könings, Ginsburg & van der Vleuten, 2018), the authors set out 4 domains that need to be considered when creating a feedback culture.
Click here for the full article
Access these other articles on feedback by clicking on the titles:
Students should be encouraged at all times to reflect on their clinical experiences and learning, so as to identify learning needs and growth areas.
Click here to watch a video explaining Reflective practice
There are many reflection models to assist with meaningful reflective practice. Some more commonly used models are:
- Rolfe’s reflective model:
What happened, what have I learned from the experience, what will I do differently in the future.
- Kolb’s reflective cycle:
- GIBBS reflective cycle: