Management of Osteochondromatosis
Osteochondroma
Click on image to view this Screencast video. This talk was given in the AOTC in september 2012
 Ostochondomas begin growth in childhood and end growing at skeletal maturity. They are situated in the metaphysis. The base consists of normal trabeculated bone and may be broad based (sessile) or narrow-based (pedunculated). The bony outgrowth is capped with a cartilage cap which is usually less than 1cm in height.
Ostochondomas begin growth in childhood and end growing at skeletal maturity. They are situated in the metaphysis. The base consists of normal trabeculated bone and may be broad based (sessile) or narrow-based (pedunculated). The bony outgrowth is capped with a cartilage cap which is usually less than 1cm in height.
Multiple Osteochondromatosis
Multiple heredity osteochondromatosis (HME) is an autosomal variant of this lesion. This form can result in growth disturbances, such as bowing of the forearms and varus and valgus deformities about he knees.
Age of presentation and distribution
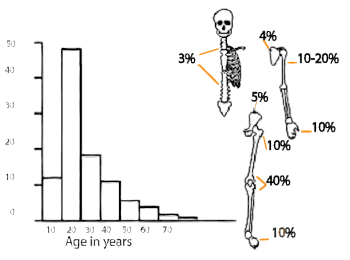
Osteochondromas form while a child is actively growing. They usually present to the doctor in the second and third decades.
The lesions are usually found at a long bone metaphysis, particularly about the knee.
They can occasionally afflict the spine, ribs and pelvis, as seen in the chart.
Associated syndromes
Metachromatosis
Is a form of the disease characterized by:
- Multiple metaphyseal juxtaepiphyseal exostoses, Metaphyseal enchondromas, periarticular calcifications, and frequent unilateral or bilateral Legg-
- Calv'e-Perthes-like changes in the femoral head, resembling Osteonecrosis.
- Cartilginous malignant change can occur in this rare syndrome.
Mavrogenis has described a case of chrondrosarcoma originating in one of these lesions.
Histology
Histologically an osteochondroma consists of a cartilage cap (there should be no mitotic cells). This is underlain by normal trabecular bone.
Imaging
Plain x-rays will show a bony outgrowth, either with a narrow or broad base. Other secondary deformities such as bowing of the forearm and varus or valgus angulation should be looked for. The cartilage cap is usually not well visualised on plain x rays and additional imaging, such as CT scan or MRI are often needed.
Pitfalls
 Anatomical variants such as the supracondylar process (Ligament of Struthers attaches to this) may be confused with an osteochondroma.
Anatomical variants such as the supracondylar process (Ligament of Struthers attaches to this) may be confused with an osteochondroma.
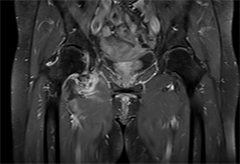
MRI
MRI is the optimal method to evaluate the thickness of the cartilage cap (less than 1cm). The presence of osteochondromatosis in this patient was found incidentally after x rays for a gunshot injury.
There are many such 'inactive' cases of MO in the community and the real incidence of complications is probably much less than quoted in literature based on operated cases.
Normal anatomical variations such as the large supracondylar process on the left may be mistakenly interpreted as an osteochondroma.
Isotope scans
- PET Scans
- Purandare found these were a good indicator of malignant change
- Yearly isotope scans are recommended for follow up in Multiple Osteochondromatosis.
Deformities seen in Multiple Osteochondromatosis
- Multiple Osteochondromas
- Hereditary multiple exostosis
- Diaphyseal aclasis
- Shortening ulna Bowing of radius (39-60%)
- Limb inequality (10-50%)
- Varus knee (8-33%)
- Short Stature
Multiple Osteochondromas (hereditary multiple exostoses, diaphyseal aclasis) are characterized by the presence of multiple osteochondromas the number of which can vary significantly between and within families. Most Multiple Osteochondroma patients also suffer from a variety of orthopaedic deformities like shortening of the ulna with secondary bowing of the radius (39-60%), inequality of the limbs (10-50%),varus or valgus angulation of the knee (8-33%), deformity of the ankle (2-54%) and disproportionately short stature. It has been a matter of debate whether these deformities are a result of skeletal dysplasia or a result of local effects on the adjacent growth plate caused by developing osteochondromas.
A family history is important. The genes have various degrees of expression. The (causative)EXT genes can be tested for in the peripheral blood.
Causes of pain
Impingement
 Because of its position in the metaphysis, an osteochondroma can cause pain by impinging on soft tissue structures such as ligament or nerve.
Because of its position in the metaphysis, an osteochondroma can cause pain by impinging on soft tissue structures such as ligament or nerve.
Fracture
An osteochondroma with a narrow neck can fracture.
Malignant change
A more sinister cause of pain is the development of malignant change in the lesion.
Risk for malignancy (Dootjes):
- >8mm cartilage cap
- Volume >175 cm3
- Number of lesions
- Multiple 5-25%
- Single <1%
Dootjes studied 64 cases and found risk factors for conversion to a chondrosarcoma were large tumour volume and a cartilage cap > 8mm. Dootjies conclusions were "Clinical symptoms (pain and growth) are non reliable indicators for malignancy. In MO patients a cartilage-cap thickness larger than 8mm or a tumour-volume larger than 175cm3 should be considered malignant. Lower thickness of the cartilage cap than earlier reported and volume measurement both based on MRI, are indicators for malignant degeneration and should be implemented in screening protocols. "
Malignant change is mainly to chondrosarcoma. Rarely osteochondromatosis change can take place.
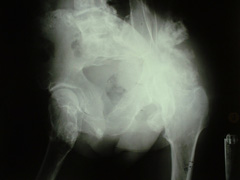 |
| This 30 year old female with multiple osteochondromatosis experienced pain over her left pelvic wing. Note the "popcorn" calcifications offer the ileal wing. The lesion is ill defined here as opposed to the sessile osteochondromas over her proximal femurs. |
Problem areas
 |
| Osteochondroma of the distal fibula |
The distal fibula is a common site. An Osteochondroma here is painful as it rubs against the tibia. An operative approach involving fibular osteotomy is recommended.
 |
| Osteochondroma of inferior acetabulum. This was excised by an ilioinguinal approach. |
Growth Deformities
 |
| Osteochondromas of both radius and ulna |
Patients with multiple enchondromatosis often develop growth deformities due to their condition.
Common deformities are varus and valgus deformities at he knee and bowing of the forearm. The radius bows because it is tethered by a shortened ulna.
Treatment of a bowed forearm ranges from excision of the tether at the distal ulna to osteotomies and straightening with an ex fix. Simple excision of the osteochondroma will give a better cosmetic result, but will not halt the progression of the disease.
Management
Symptomatic lesions should be excised.
Follow-up of Multiple osteochondromatosis
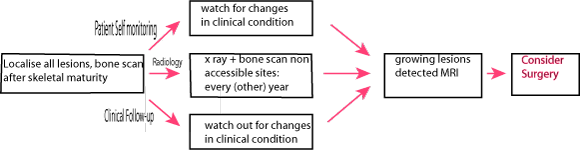 |
| Suggested follow up algorithm for Multiple Hereditary Osteochondromatosis |
Children seldom develop malignant change. Hameeltman considers it only necessary to follow patients with multiple osteochondromatosis up after skeletal maturity. After this Tc scans every alternative year are necessary if the patients have lesions in inaccessible spots.
References
- Purandare NC et al. Integrated PET/CT in evaluating sarcomatous transformation in osteochondromas. Clin Nucl Med. Jun 2009;34(6):350-
- Dootjes ,JBJS 94-B, 2012
- Shin E. W., Treatment of multiple enchondromas in children. JBJS 2006, 88-B, Pages 255-260.
- Roach, J. W.; Klatt, J. W. B. & Faulkner, N. D. Involvement of the Spine in Patients with Multiple Hereditary Exostoses J Bone Joint Surg Am, 2009, 91, 1942-1948
- Hameetman, L. Multiple Osteochondromas: Clinicopathological and Genetic Spectrum and Suggestions for Clinical Management Hered. cancer clin. pract., 2004, 2(4), 161-173