Management of malignant Pelvic Tumours
Overview
Malignant tumours of the pelvis generally present late. They are usually asymptomatic early on and later the patient presents with vague visceral pain. Cachexia and other late signs are not common with these tumours.
Physical Examination
Besides palpating the mass particular attention should be given to:-
- Rectal and vaginal exam -especially if the sacrum is involved.
- Neurological examination - Is there fallout and are the sacral roots involved?
Imaging
Standard X rays including oblique views are standard. CT and or MRI are good for visualising soft tissues. Use of contrast may enhance visualisation of viscera.
Angiography is useful especially with internal hemipelvectomy to visualise the level of common iliac bifurcation. Preoperative embolization via this method is also used to decrease bleeding intra-operatively.
In addition Sigmoidoscopy and colonoscopy may be needed to determine if the bowel is invaded with tumour.
Anatomical considerations
The iliacus muscle is a barrier to spread of tumours of the ilium bone. Tumour breakthrough can occur anteriorly along the pelvic brim and posteriorly into the sciatic notch. for anatomical reasons tumour is more likely to invlove pelvic viscera on the left side. The aorta bifurcates at L4 and arteries are anterior to their corresponding veins.
Another place where vessels are at risk of tumour invasion is near the ischiopubic rami. Here the urethra is also at risk of tumour infiltration.
Surgical considerations:
Hemipelvectomy
Conventional hemipelvectomy is an operation where half of the pelvis and the ipsilateral lower limb is removed.
Reasons for doing this operation include:-
- Massive thigh and pelvic tumours
- Large sarcomas of the pelvis
- Massive pelvic trauma
- Uncontrollable pelvic sepsis
Types of Hemipelvectomy
 |
| Hemipelvectomy done for recurrence of grade 2 chondrosarcoma |
Levels of Conventional hemipelvectomy
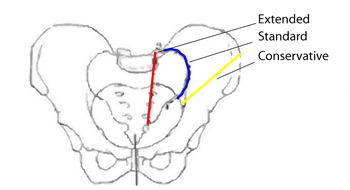 Hemipelvectomy can be is usually done by disarticulating the sacroiliac joint and then through the Symphysis pubis. If the sacral nerve roots are involved an Extended hemipelvectomy can be done at the level of the nerve roots. If the proximal ilium is not involved it can be retained, thus preserving some of the pelvic form. This procedure is known as a Conservative hemipelvectomy.
Hemipelvectomy can be is usually done by disarticulating the sacroiliac joint and then through the Symphysis pubis. If the sacral nerve roots are involved an Extended hemipelvectomy can be done at the level of the nerve roots. If the proximal ilium is not involved it can be retained, thus preserving some of the pelvic form. This procedure is known as a Conservative hemipelvectomy.
 |
| Conservative hemipelvectomy done for Ewing's sarcoma of the proximal femur also involving the pelvis |
Limb sparing partial pelvectomies
If the limb itself is not involved and in good shape, a limb sparing partial pelvectomy may be feasible. The Internal hemipelvectomy has 3 types described by Enneking.
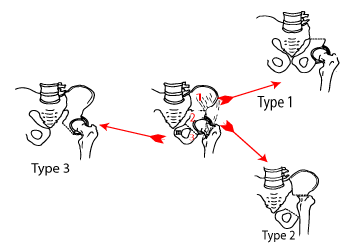
Types of pelvic resections
- Type 1 - Ilium is resected
- Type 2 - Acetabulum is resected
- Type 3 - Ischiopubic rami are resected
If the general condition of the limb is good and a good tumour free margin can be achieved, an internal hemipelvectomy can achieve as good an oncological outcome as external hemipelvectomy.
Advantages of internal hemipelvectomy
- Margins the same as classical hemipelvectomy can be achieved
- A functional limb can be preserved
- Life expectancy can be reasonable
Contraindication to limb sparing surgery
- Recurrence
- Where sacral nerve roots are involved
- Extension of tumour into the thigh
- Poor physical condition
- Poor circulation in the limb e.g. atherosclerosis
 |
.jpg) |
 |
| Ewing's Ilium in a 9 year old girl | After a Type 1 resection and arthrodesis hip | Correcting the growth inequality 2 years later |
Type 2 resections
Here the acetabulum, and it's weight transfer function from the lower limb must be replicated.
Solutions include:
- Arthrodesis either ischiofemoral or between femur and remaining ilium.
- Bone replacement either allograft femur (a proximal femur has almost the same shape as the brim of the true pelvis, or autograft from the same femur taken during hip arthroplasty. A total hip replacement is then done inserting the acetabular component into the graft. The grafted acetabular substitute needs secure internal fixation with plates and screws and non union is common.
- Prosthetic replacement: The traditional replacement was the saddle prosthesis which was 'Y' shaped extension of the proximal femur to allow the device to straddle the remaining Ilium. Prosthetic replacements for the missing piece of acetabular pelvis are recently available.
Type 3 resections:
With these weight bearing is not needed, but the challenge is neurovascular involvement. The external iliac / femoral vessels are often involved as is the urethra. Careful imaging with M. R.I. and other studies is required to determine if these structures are infiltrated, in order to make the decision as the whether they are resectable.
Metastases
To increase quality of life there is sometimes there an indication for hemipelvectomy with pelvic metastases.
When to operate
- Failure of conservative treatment
- Patient refractory to chemo or radio therapy
- Reasonable expectancy of survival for more than a few months
Techniques
The idea is to restore the weight bearing capacity of the acetabulum and then do a total joint replacement.
Tumour is curetted out of the (superior) acetabulum and the defect replaced by bone cement or bone graft.. Radioscopic embolization may also be used to decrease tumour size.
Also consider embolization especially in renal metastases. The Acetabular defect is then addressed with the same principles as a ‘protrusio hip’ or other defective acetabulum needing a total hip replacement. This principle is to transmit weight bearing forces to the spine. Bony deficiencies have to be addressed in this load bearing area. Marco used a prortusio cup, and total hip replacement in 3 cases, the rest he cemented using screws as in the example above. (Total 54 Cases)
Patients with pelvic metastases have a poor life expectancy. Marco considers that internal hemipelvectomies will give these people good palliation. A very robust reconstruction is not necessary because of their decreased life expectancy.
References
- Malawer M.: Operative techniques in orthopaedic surgical oncology. Le Roux, T.; Resection of pelvic tumours – Hemipelvectomy or Internal Hemipelvectomy, JBJS 2005, 87-B, 279-280
- Marco, R.,Functional and oncological outcome of acetabular reconstruction – metastatic,JBJS, 2000, 82-A, 642
- Delloye, Pelvic Reconstruction with a Structural Pelvic Allograft After Resection of a Malignant Bone Tumor,JBJS, 2007, 89, 579-587
- Pring, M. Chondrosarcoma of the pelvis: A review of 64 cases JBJS, 2001, 83-A, 1630
- Biau, D. J., Ipsilateral Femoral Autograft Reconstruction After Resection of a Pelvic Tumor JBJS, 2009, 92-A, 142-151
- Carter, S. R. Hindquarter amputation: Is it still needed and what are the outcomes? Bone & Joint Journal, 2013, 95-B, 127-131